Scleral Contact Lenses
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.


Overview
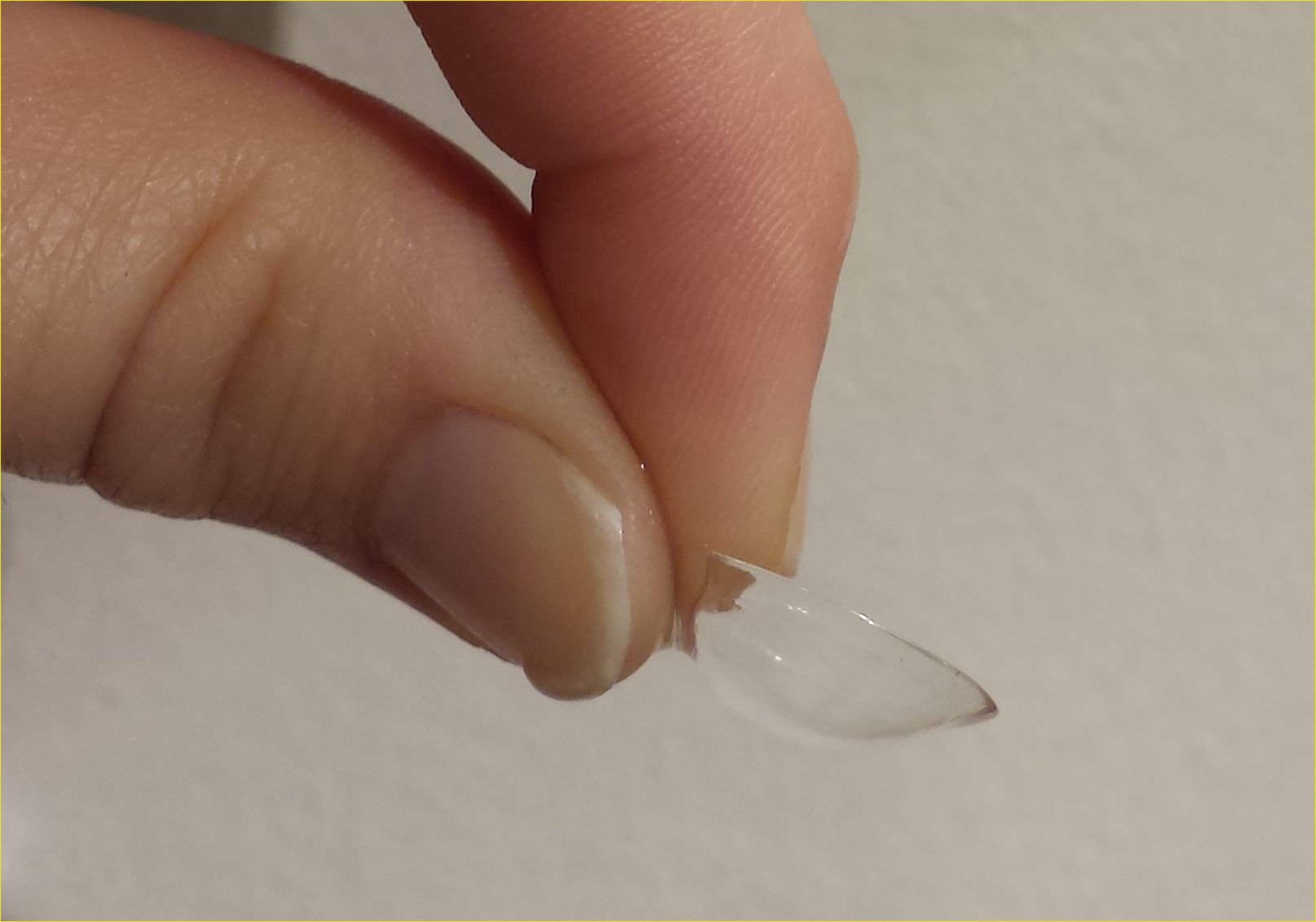
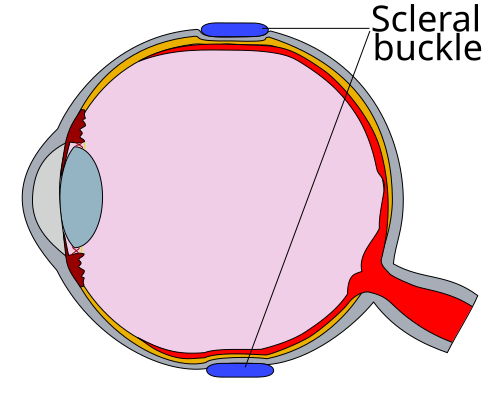
Scleral contact lenses are large, rigid gas-permeable lenses that rest on the white part of the eye (sclera) and vault over the clear front window (cornea). This creates a gentle “fluid bath” between the lens and the eye that can protect the surface and sharpen vision in people whose corneas are irregular or very sensitive. 1 Because the lens sits on the sclera (which has fewer nerve endings than the cornea), many people find these lenses comfortable once they learn insertion and care. 2
People try scleral lenses for different reasons—such as keratoconus, post-LASIK ectasia, or very dry/fragile corneas. When a scleral lens vaults over the cornea, the fluid reservoir can smooth the optical surface and keep it moist during the day. With the right fit and care, many wearers enjoy stable vision for work, school, and sports.
How the Procedure Works & Options
How fitting works: A cornea/contact lens specialist measures your eye shape and maps your cornea. A trial (diagnostic) scleral lens is placed and allowed to settle for 20–30 minutes. The doctor checks the vault (space under the lens), the edges (landing zone), and vision—repeating with small design changes until the lens clears the cornea evenly, lands gently on the sclera, and provides crisp vision. 3 Scleral lens fitting is hands-on and may take a few visits, especially for complex eyes.
Sizes & design options:
- “Mini-sclerals” ≈ 14–18 mm; larger designs up to ~24 mm.
- Toric or quadrant-specific landings for non-round eyes.
- Front-surface toric optics for astigmatism; multifocal optics for reading.
- Notches to avoid bumps; tints for light sensitivity.
- Wavefront-guided optics may be considered later if glare/halos persist. 4
Who Is a Candidate?
Often good candidates:
- Irregular corneas (keratoconus, pellucid marginal degeneration, post-LASIK ectasia) and post-transplant eyes.
- Severe dry eye or ocular surface disease (e.g., GVHD).
- High prescriptions hard to correct comfortably with standard lenses. 5
- Patients able to manage daily care steps. 6
Who may need a different plan: People unable to manage daily cleaning/insertion/removal, or with active infection or uncontrolled allergy. Your clinician may treat eyelid/tear film issues first so lenses stay clear and comfortable.
Scleral Lens Suitability Score
Select your details to estimate suitability.
Benefits and Limitations (Plus Costs & Pricing)
Benefits:
- Sharp, stable vision by masking an irregular cornea.
- Often all-day comfort—lens rests on the sclera.
- Fluid reservoir can shield fragile surfaces and reduce irritation. 7 8
Limitations:
- Fitting takes time/expertise and multiple visits.
- Learning curve for insertion, removal, and hygiene.
- Possible “midday fogging” (debris under lens) requiring a quick rinse/refill; poor hygiene can lead to infection. 9 10
Cost & price (what to expect): Fees are often packaged (fitting/imaging, custom lenses, training, early adjustments). For insurance queries, practices may reference HCPCS codes for scleral lenses—V2531 (scleral, gas-permeable, per lens) and V2530 (scleral, gas-impermeable, per lens)—but coverage varies by plan and medical necessity. 11 12
Smart budgeting tips:
- Ask for a written, itemized estimate (services, lenses, follow-ups, remake policy).
- Check medical/vision benefits for “medically necessary” coverage and needed documentation.
- Use HSA/FSA funds if eligible; ask about payment plans.
- Plan for replacements and yearly fit checks.
Risks and Side Effects
Most side effects are preventable with careful fit and hygiene. Common issues include midday fogging (debris in the reservoir), tiny bubbles from incorrect insertion, mild temporary corneal swelling after long wear, and occasional lens suction on removal. Your provider can adjust vault, edge shape, and care routine to reduce these problems. 13 Serious infections are uncommon but can threaten sight—never sleep or swim in lenses unless your doctor approves, and keep lenses/solutions away from tap water. 14
Call the clinic right away for:
- Eye pain, redness, light sensitivity, or discharge.
- Sudden blurry vision. Remove the lens and contact your eye-care team.
Recovery and Long-Term Care
Learning curve: Most people adapt within 1–2 weeks. Typical steps: wash/dry hands; rinse lens with GP solution; fill the bowl with preservative-free saline; look down into a mirror and gently place using an insertion plunger; later remove with a small suction cup (remover). Your specialist will provide written instructions to avoid bubbles and edge awareness. 15 16
Everyday habits that help:
- Use products recommended for scleral lenses; never use tap water.
- Replace solution each time—do not “top off.”
- Rinse and air-dry the case daily; replace the case at least every 3 months.
- Take brief screen breaks and blink fully to reduce dryness.
- Schedule yearly fit checks, or sooner if comfort/vision changes.
Latest Research & Innovations
Modern high-oxygen (high-Dk) mini-scleral lenses show small average corneal swelling after a typical day of wear (often < 2%), suggesting safe oxygen delivery when lenses and reservoirs are well designed. 17 Tools like corneal-scleral profilometry and quadrant-specific landings help customize the edge for comfort and tear exchange. 18
Optics on the cutting edge: Wavefront-guided (WFG) scleral lenses can reduce higher-order aberrations that blur vision even with a great standard fit—improving night vision, contrast, and satisfaction in selected eyes. 19 Many clinics consider WFG after a stable fit and easy routine care. 20
Recent Peer-Reviewed Research
Intracorneal Hemorrhage Associated With Scleral Lens Wear.
Trinh J, Bernhisel AA, Nau CB, et al.
Intraocular pressure following long-term scleral lens wear in Chinese eyes.
Yang M, Wang F, Xu A, et al.
Profilometry-Guided Scleral Lenses Improve Visual Acuity and Reduce Ocular Aberrations in Irregular Corneas: A Retrospective Case Series.
Barone V, Petrini D, Surico PL, et al.
Next Steps
If you have an irregular cornea, severe dry eye, or trouble with regular contacts, consider an evaluation with a cornea & contact lens specialist. Bring your glasses, current lenses (if any), eye-drop list, and a short note about your goals (work, sports, night driving). Ask about expected number of visits, training, warranties, and the plan if lenses fog midday. 21 You can also review safe-wear tips now so you’re ready to get the most out of your fit. 22
Reminder: This page is for education only and does not replace in-person care. Your specialist will tailor the lens and care routine to your eyes and lifestyle so you can see comfortably and safely day to day.
Trusted Specialists
Board-certified providers specializing in Scleral Contact Lenses.








