Salzmann Nodular Degeneration
Last updated September 6, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
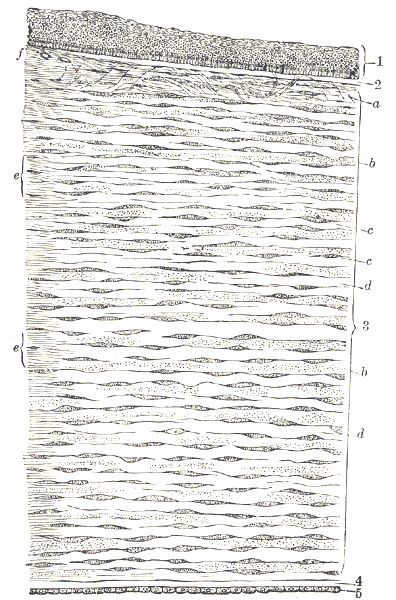
Salzmann nodular degeneration (SND) is a corneal condition where small, raised, gray-white to bluish nodules form on the cornea. These lie just under the epithelium and over Bowman’s layer. SND can be quiet for years, or it can cause irritation, irregular vision, and trouble getting glasses to work well. It often affects both eyes and usually develops slowly. 1
Long-term surface irritation, prior eye surgery/trauma, and dry eye or lid inflammation may contribute. Small peripheral nodules may be asymptomatic; larger or central ones can blur vision or increase glare. Treatments range from lubrication and lid care to superficial keratectomy or PTK laser smoothing when vision is affected. 2
Symptoms
Many people notice few symptoms at first. As nodules enlarge or move centrally, you might have:
- Blurry or fluctuating vision, often worse with dryness
- Glare/halos, especially at night
- Foreign-body sensation, burning, or tearing
- Astigmatism changes that make glasses or contacts less effective
Some are diagnosed on routine exam when classic raised nodules are seen. Large or central nodules can distort the corneal surface and reduce vision, which may improve after treatment. 1 4
Causes and Risk Factors
The exact cause is unknown, but SND likely develops when the corneal surface is chronically stressed, triggering scar-like tissue beneath the epithelium. Common links include:
- Chronic surface irritation: dry eye, blepharitis/meibomian gland dysfunction
- Prior surgery or inflammation (e.g., pterygium surgery, long-standing keratitis)
- Contact lens wear or prior trauma
- Demographics: reported more often in women and in midlife (can occur at many ages)
These factors do not cause SND in everyone but may raise the chance that nodules form or recur. 2 4
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
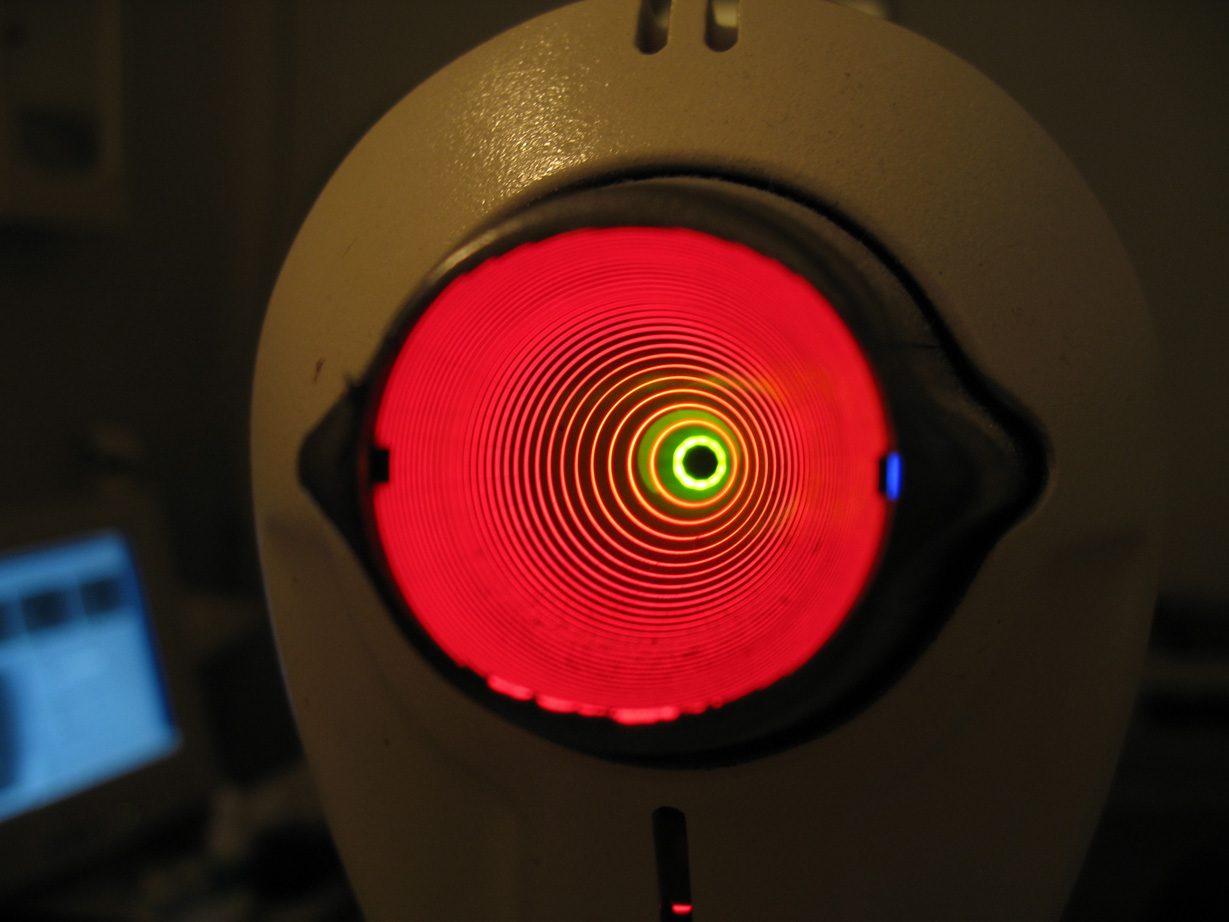
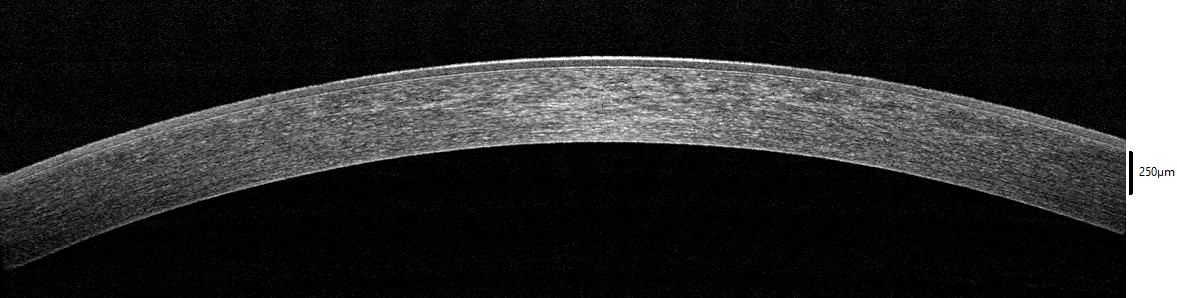
Doctors diagnose SND at the slit lamp by identifying elevated bluish-white subepithelial nodules. Typical testing includes:
- Vision/refraction to assess impact on sight
- Slit-lamp exam to locate/measure nodules and assess dryness/lid disease
- Corneal topography/tomography to map shape and irregular astigmatism
- Anterior segment OCT to gauge nodule depth and Bowman’s layer changes
These help decide on observation vs. treatment and track changes after intervention. 1 5
Treatment and Management
Treatment aims to smooth the surface, reduce irritation, and improve vision. Plans depend on symptoms, nodule size/location, and optical impact.
- Medical care first: frequent lubricants, lid hygiene, warm compresses, dry eye therapy; short topical anti-inflammatory courses in select cases
- Superficial keratectomy (SK): gentle removal/polishing of nodules for rapid comfort/vision improvement when prominent
- Phototherapeutic keratectomy (PTK): laser smoothing for residual irregularity or recurrence; many patients gain vision and more regular curvature 7
- Mitomycin-C (MMC): brief intraoperative use with SK/PTK in selected cases to reduce scarring/recurrence 8
- Corneal grafting (rare) for deep disease or persistent visual loss
Aftercare: bandage contact lens plus antibiotic/anti-inflammatory drops are common. Vision and corneal shape are rechecked over weeks–months, especially before cataract surgery (SND can affect biometry). 6
Living with Salzmann Nodular Degeneration and Prevention
Most people do well with steady care. Helpful habits:
- Care for the surface: use artificial tears as directed; treat dry eye and lid disease
- Protect the cornea: avoid eye rubbing; use protection in dusty/windy settings
- Follow your plan: keep follow-ups; repeat topography/OCT as advised
- Plan around surgery: consider treating central nodules before cataract biometry
There is no sure prevention, but controlling surface problems can reduce irritation and may lower formation/recurrence risk. 4
Latest Research & Developments
Why some nodules recur: Myofibroblasts and epithelial–Bowman’s layer interface changes may underlie difficult or recurrent SND, explaining why some nodules don’t simply scrape off. 3
Laser outcomes: PTK (often after SK and sometimes with MMC) can improve vision and surface regularity; technique is individualized and refractive shifts monitored. SND can affect cataract measurements; treating nodules first may improve accuracy. 9
Recently Published in Peer-Reviewed Journals
Cornea
June 1, 2024
Manual Superficial Keratectomy Is the First Choice Treatment for Salzmann Nodular Degeneration.
Scorsetti MM, Eguiza VS, Durán JA
BMC ophthalmology
March 12, 2022
Salzmann nodular degeneration in posterior keratoconus: a case report.
Song P, Yu X, Pang C
Cornea
February 1, 2022
Peripheral Hypertrophic Subepithelial Corneal Degeneration.
Raber IM, Eagle RC Jr
Next Steps
If you have SND—or notice new blur, glare, or irritation—book a visit with a cornea specialist (ophthalmologist). Bring your glasses/contact prescription, list of drops, and prior eye records.
- Scheduling tips: ask for a “cornea evaluation”; request the cancellation list if waits are long; obtain referrals if your plan requires them
- What to expect: topography, OCT, and slit-lamp exam; if nodules are central/bothersome, superficial keratectomy with/without PTK may be discussed
- Quick education: Kerbside can help you prepare (informational only; not a physician–patient relationship)
Many patients do very well with treatment and steady surface care. Your specialist will help time SND care around any planned cataract or corneal surgery. 4