Dry Eye Treatments
Also known as Dry Eye Therapy
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms for details.



Overview
Dry eye disease (DED) happens when your eyes do not make enough healthy tears or the tears evaporate too fast. The surface of the eye becomes dry and irritated, causing burning, stinging, a gritty or sandy feeling, light sensitivity, and blurry or fluctuating vision—often worse with long screen time or in dry, windy rooms. Dry eye is common at all ages, increases with aging, and is more frequent after menopause in women. Most people feel much better with the right plan. 1
Treatments range from simple self-care (artificial tears, warm compresses, eyelid hygiene, smart blinking) to prescription medicines that calm inflammation or boost tearing, and office procedures that help eyelid oil glands work better. Care is tailored to your symptoms, exam findings, and goals using a stepwise approach recommended by professional guidelines. 2
How the Procedure Works & Options
Your treatment plan is layered and customized. Most people start with over-the-counter artificial tears used several times daily. If dryness continues, your eye-care professional may add prescription therapies or in-office options based on the type of dry eye (aqueous-deficient, evaporative from meibomian gland dysfunction, or mixed).
- Artificial tears, gels, ointments: relieve symptoms and protect the surface. Preservative-free is best if you dose very often.
- Prescription drops: cyclosporine helps your own glands make more tears by reducing surface inflammation; lifitegrast targets inflammatory pathways.
- Nasal spray to stimulate tears: varenicline nasal spray can increase natural tearing for some people. 6
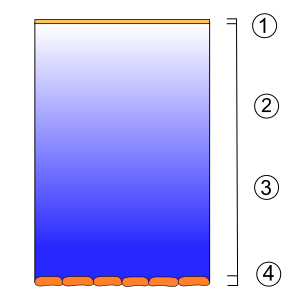
- Punctal plugs: tiny silicone plugs placed in the tear drain openings to keep natural tears on the eye longer.
- Lid-based care for oil glands: warm compresses and eyelid cleansers at home; in-office thermal pulsation or intense pulsed light (IPL) for selected patients with meibomian gland dysfunction.
Your clinician will mix and match options, and adjust them over time, to keep you comfortable and protect the ocular surface. 3
Who Is a Candidate?
You may benefit from professional dry eye care if you have daily symptoms for weeks, rely on screens for school or work, wear contact lenses, live in a dry climate, or have conditions like blepharitis, rosacea, or autoimmune disease (e.g., Sjögren’s). People after LASIK/PRK, those taking certain medicines (antihistamines, some antidepressants), and post-menopausal women are also at higher risk. 1
A clinic visit confirms the type and severity with tests such as tear volume, tear breakup time, ocular surface staining, and meibomian gland evaluation. Based on these findings, your doctor will build a stepwise plan. Many people do well with a combination of tears, eyelid care, and targeted prescriptions; others may add punctal plugs or in-office gland treatments for more lasting stability. 2
Dry Eye Suitability Score
Select your details to estimate suitability.
Cost and Price
What to expect (U.S.). Costs vary with the type of therapy. Over-the-counter artificial tears are usually the least expensive (often a few dollars per week). Prescription medicines (cyclosporine, lifitegrast, varenicline nasal spray) are filled at a pharmacy and may be covered under Medicare Part D or commercial drug plans—coverage rules and copays differ by plan.
- OTC care: preservative-free tears cost more per vial but are gentler if you dose ≥ 4×/day.
- Prescription drops/sprays: ask about formulary tier, prior authorization, and 90-day fills; some medicines have manufacturer programs.
- Punctal plugs & office procedures: may or may not be covered; clinics can provide an estimate for plugs, thermal pulsation, or IPL and any follow-ups. 7
Smart budgeting tips: request an itemized quote (visit, testing, procedures), bring insurance details to check coverage, and track indirect costs (missed work, repeated product purchases). Dry eye can create meaningful costs, so effective therapy may offset some of the burden over time. 8
Benefits and Limitations
Benefits when dry eye is controlled: clearer, more comfortable vision for reading, screens, and driving; fewer flares of redness/irritation; and better protection of the corneal surface. Many people notice steady gains over the first 4–8 weeks as the tear film stabilizes and the surface heals. 1
Limitations to keep in mind: dry eye is usually chronic. You may need ongoing tears and eyelid care, and some treatments (like certain in-office gland procedures) may require maintenance. Not every therapy works for every person—your team may adjust drops, add punctal plugs, or combine approaches until the balance is right. Guidelines emphasize a personalized, stepwise plan rather than “one size fits all.” 2
Risks and Side Effects
Artificial tears: generally safe. If you need drops very often, choose preservative-free to avoid irritation from preservatives.
Prescription drops: cyclosporine and lifitegrast may cause brief burning or unusual taste after instillation; remove soft contact lenses before dosing and wait 15 minutes before reinsertion (per labels). 4 5
Punctal plugs: can cause temporary watering, foreign-body sensation, or plug loss; they are removable if bothersome.
Office procedures (thermal pulsation, IPL): may lead to short-lived redness or tenderness; serious complications are uncommon in trained hands. If you have severe pain, vision change, or discharge, contact your clinic promptly.
Recovery and Long-Term Care
Short term: Lubricating drops work right away but wear off—keep them handy. Prescription medicines often need several weeks to reach full effect; stay consistent even if early changes are subtle. After plugs or in-office treatments, most people resume normal activity the same day; mild eyelid warmth or redness usually fades within hours. 3
Habits that help:
- Take blink breaks (20-20-20 rule) and use a humidifier.
- Wear wraparound sunglasses on windy days.
- Cleanse the lids gently if you have blepharitis, and stay hydrated.
- Bring your drops to visits so your clinician can simplify your regimen and avoid duplicates.
Stepwise care that treats both inflammation and tear evaporation gives the best long-term results. 2
Latest Research & Innovations
What research shows: Reviews highlight mechanism-based care that targets inflammation, restores the oil layer, and stabilizes the tear film—with growing evidence for prescription drops, nasal neurostimulation, and eyelid-based therapies in selected patients. 9
New tools: AI-assisted imaging can grade meibomian glands and tear film signs more objectively (promising but needs standardization/validation). 10 Device platforms for thermal gland therapy and IPL continue to evolve, while drug research explores more comfortable formulations and novel targets to speed relief and protect the surface.
Recent Peer-Reviewed Research
Electronic device exposure and dry eye symptoms among medical and nonmedical Palestinian university students: a multicenter cross-sectional study of associated factors.
Alashqar M, Taqatqa S, Ayaseha A, et al.
Comparison of SPEED and OSDI questionnaires for dry eye symptom in Chinese college students: a cross-sectional study.
Meng X, Geng R, Yang K, et al.
Corneal Staining Responder Analysis: A Clinically Meaningful Dry Eye Outcome.
Akpek EK, Sheppard JD, Krösser S
Next Steps
If dryness limits your work, school, sports, or driving, schedule a visit with an ophthalmologist or optometrist experienced in dry eye. Bring a list of symptoms, current drops, contact lens routine, and your environment (fans, air vents, screen hours). Ask which type of dry eye you have and whether your plan should include prescription drops, punctal plugs, or eyelid-based procedures. Evidence-based guidance helps your team build a step-by-step plan to get you comfortable again. 3 2
Note: This page is educational and does not replace medical advice. Your clinician will personalize care so you can see comfortably and protect your eye surface over the long term.