Pseudoexfoliation Glaucoma
also known as PXG
Last updated September 5, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
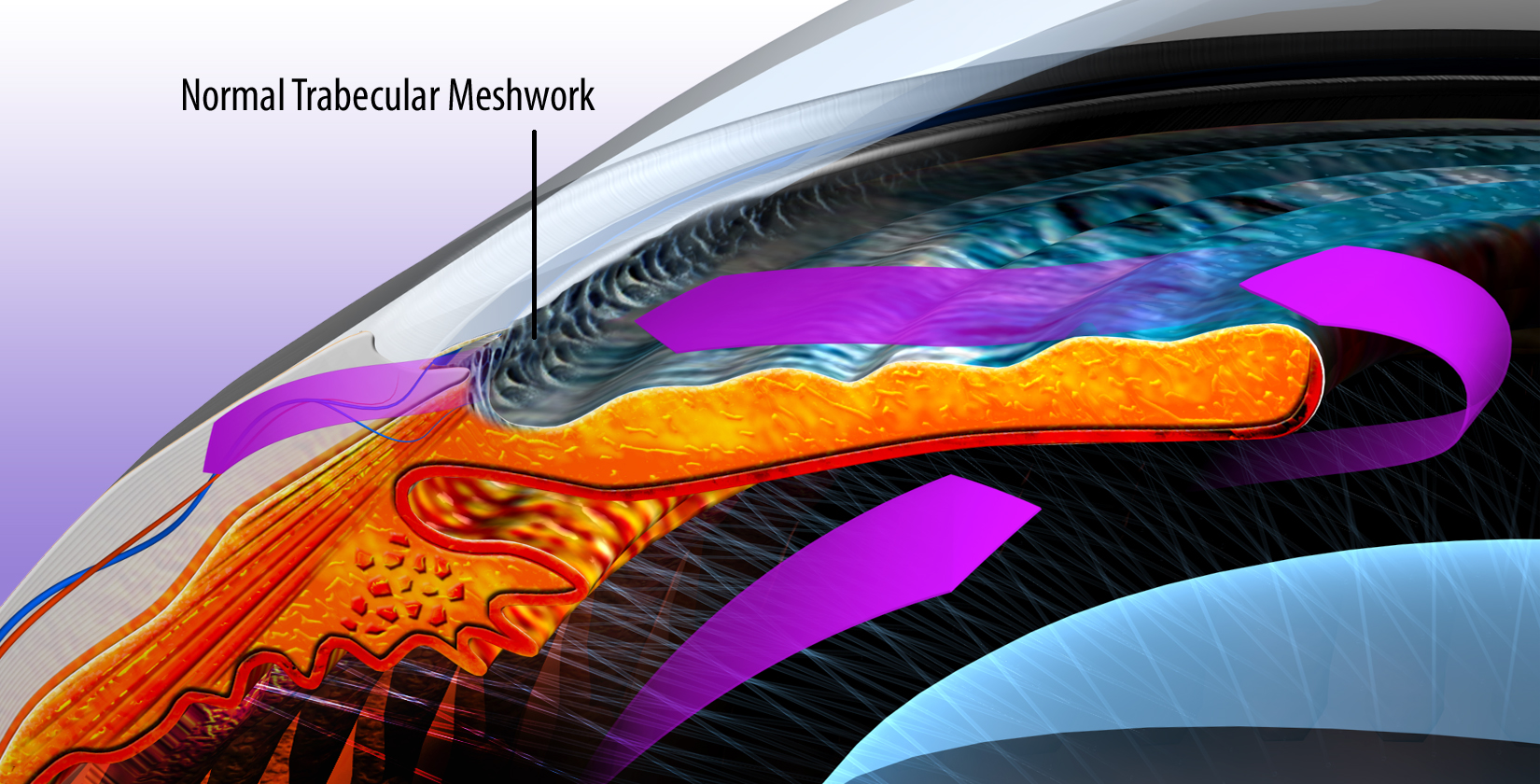
Pseudoexfoliation glaucoma (PXG) is a type of open-angle glaucoma that occurs in some people with pseudoexfoliation syndrome (PEX). In PEX, a dandruff-like protein material builds up on the lens, iris, and the eye’s drain (trabecular meshwork). This can block fluid outflow, raise eye pressure, and harm the optic nerve over time. PXG is one of the most common causes of secondary open-angle glaucoma worldwide. 1
Because the eye’s drain is open but clogged, people may not notice problems until side vision slowly fades. Regular eye exams are essential. The National Eye Institute lists exfoliation (pseudoexfoliation) glaucoma among major glaucoma types and notes that family history can raise risk. 2
Symptoms
Early on, most people feel fine and see normally. PXG usually starts without pain. Over time, untreated glaucoma can cause slow loss of side (peripheral) vision. Some people have pressure spikes, especially after eye dilation or surgery, which can blur vision for a short time.
Common clinical clues:
- White, flaky material on the front of the lens
- Poor pupil dilation
- Pigment along the eye’s drain
Testing often finds problems before you notice them. That’s why routine exams, visual fields, and OCT scans are so important. 3
Causes and Risk Factors
PXG develops in people with pseudoexfoliation syndrome (PEX), where extra protein-like flakes collect in the front of the eye. This material can clog the drain and raise eye pressure. PEX is more common with older age and is seen in many populations worldwide. 4
Risk factors include:
- Age: Risk rises after age 60.
- Family history & genetics: LOXL1 gene variants are linked to exfoliation syndrome and exfoliation glaucoma. 6
- One-eye to two-eye spread: PEX may start in one eye and appear later in the other.
- Fragile eye structures: Weaker lens “springs” (zonules) can reduce dilation and make cataract surgery more challenging. 4
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
An eye doctor (optometrist or ophthalmologist) makes the diagnosis after a full exam.
Typical steps:
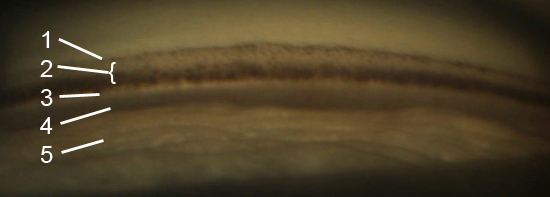
- Slit-lamp exam to spot white, flaky deposits on the lens capsule and pigment on the cornea or iris.
- Gonioscopy to examine the drainage angle for heavy pigment and a Sampaolesi line (pigment in front of Schwalbe’s line).
- Eye pressure (IOP) checks, sometimes at different times of day.
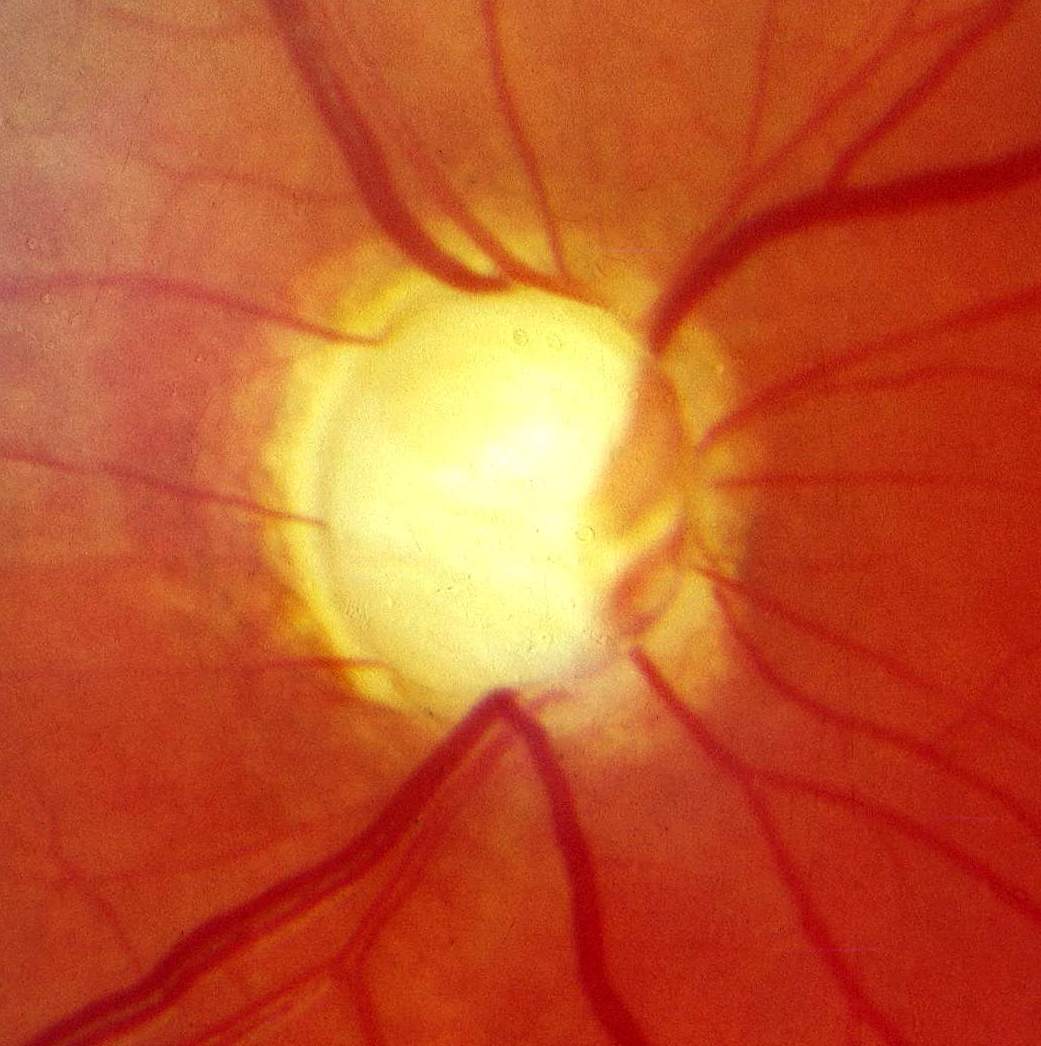
- Optical Coherence Tomography (OCT) to measure retinal nerve fiber and ganglion cell layers.
- Visual field testing to map side-vision loss.
Doctors also rule out other causes of high pressure or optic nerve damage. Compared with typical open-angle glaucoma, PXG can show higher pressure spikes and faster changes, so closer follow-up is common. 1 5
Treatment and Management
The goal is to protect the optic nerve by lowering eye pressure to a safe range. Your doctor will set a personal target based on your optic nerve, visual fields, and overall risk. Treatment often starts like other open-angle glaucomas but may need to be more assertive because PXG can fluctuate.
Options:
- Prescription eye drops: Prostaglandin analogs are common first-line medicines; beta-blockers, alpha-agonists, and carbonic anhydrase inhibitors are also used. Some people need combinations.
- Selective Laser Trabeculoplasty (SLT): Clinic laser that helps the drain work better; used as first-line or add-on therapy and can reduce daily drops. 8
- Surgery: If progression or pressure spikes persist, procedures such as trabeculectomy, glaucoma drainage implants, or MIGS may be recommended. Lens weakness in PEX can influence surgical planning.
- Cataract surgery considerations: PEX eyes may dilate poorly and have weaker lens support; surgeons may use capsular tension rings and other devices to keep surgery safe. 7
Costs & price (practical tips):
- Ask for generics when possible; 90-day supplies, discount cards, or manufacturer programs can lower costs.
- SLT is usually outpatient—request a pre-estimate listing surgeon, facility, and professional fees; confirm deductible/coinsurance.
- Surgery costs vary by facility, anesthesia, implants, and surgeon—ask for a bundled quote and confirm in-network status; ask about payment plans if you have a high-deductible plan.
- Testing (OCT, visual fields) is typically covered when medically necessary; verify frequency limits.
Daily habits that help: Use drops exactly as prescribed, bring bottles to visits, keep all follow-ups, avoid smoking, and discuss safe exercise plans if you’ve had pressure spikes after dilation or strenuous activity. 1
Living with Pseudoexfoliation Glaucoma and Prevention
PXG is lifelong, but many people keep good vision with consistent care.
Simple steps:
- Stick to treatment: Set phone reminders and link drops to a routine (e.g., brushing teeth).
- Don’t skip checkups: Visual fields and OCT scans catch small changes early.
- Share your full medication list (including over-the-counter) with your eye team.
- Plan for procedures: Tell your surgeon if you have PEX; it can affect cataract surgery choices and supports used during the operation. 7
There’s no sure way to prevent PEX or PXG, but early diagnosis and steady pressure control greatly lower the risk of vision loss. See the NEI overview of glaucoma types and treatments for more. 2
Latest Research & Developments
Genetics (LOXL1): Research continues to confirm strong links between LOXL1 variants and exfoliation syndrome/glaucoma; work is ongoing to understand elastic fiber biology and potential targeted therapies. 6
Less-drop care: Reviews and trials support SLT as a first-line option for many with open-angle glaucoma—useful in PXG, where adherence to multiple drops can be difficult and pressure may fluctuate. 9
Other active areas include why pressure spikes are more common in PXG, protecting the optic nerve, and making surgery safer for eyes with weak lens support. 5
Recently Published in Peer-Reviewed Journals
American journal of ophthalmology
August 7, 2025
Predictors of Glaucoma Conversion in an African Ancestry Cohort: A Longitudinal Study.
Zhao AT, Rosa ID, Salowe R, et al.
Ophthalmology. Glaucoma
July 26, 2025
Selective Laser Trabeculoplasty and the Evolving Glaucoma Paradigm.
Realini T, Gazzard G
BMC ophthalmology
July 23, 2025
Analysis of surgical outcomes and risk factors after gonioscopy-assisted transluminal trabeculotomy.
Gunay M, Turk A, Kurutas OK, et al.
Next Steps
If you have PEX or PXG, the best specialist to see is a glaucoma specialist (ophthalmologist). Many people start with an optometrist or general ophthalmologist and are referred as needed.
How to schedule:
- Ask for a “glaucoma evaluation.”
- Bring your glasses or contact lens info, medication list, and prior eye records.
- If your insurance needs a referral, call your primary care clinic first.
Timing tips: Ask to be added to a cancellation list. If you’ve noticed sudden blur or halos after dilation or strenuous activity, tell the scheduler to aim for a sooner visit.
Fast guidance: You can connect with the right specialist on Kerbside for a medical education consult to prepare for your visit (educational only; no physician–patient relationship). For a plain-language overview of glaucoma types and treatments, see NEI’s resource. 2


