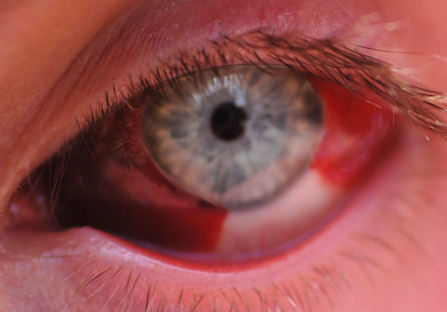
Subconjunctival Hemorrhage
Last updated August 5, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.



Overview
A subconjunctival hemorrhage happens when a tiny conjunctival blood vessel ruptures and leaks blood onto the white of the eye (sclera). The result is a dramatic red patch that often looks worse than it feels. Most episodes follow a sudden increase in venous pressure—such as during coughing, sneezing, straining, or vigorous eye-rubbing—and clear on their own in one to three weeks without harming vision.1 Because the conjunctiva is transparent, the blood is trapped beneath it and cannot be wiped away. Although alarming, the condition is usually benign; rare cases signal systemic bleeding problems or ocular trauma and warrant specialist care.2
Symptoms
Unlike most red-eye disorders, a subconjunctival hemorrhage is painless and does not blur vision. Typical features include:
- Bright-red, sharply bordered patch on the sclera—usually in one sector.3
- No discharge, itching, or light sensitivity.
- Mild scratchy sensation or awareness of eye fullness in some people.4
- Color change over time: red ➜ maroon ➜ yellow-green as blood is resorbed.
Warning signs such as pain, recurrent bleeding, or simultaneous skin bruising suggest an underlying systemic or traumatic cause and should be evaluated promptly.
Causes and Risk Factors
Most bleeds occur spontaneously, yet several factors increase risk:
- Valsalva maneuvers: coughing, heavy lifting, vomiting, or childbirth.1
- Systemic hypertension and diabetes, which make vessels fragile.2
- Blood thinners (aspirin, warfarin, direct oral anticoagulants) or platelet disorders.4
- Ocular trauma or surgery, including LASIK and eyelid procedures.3
- Advanced age (≥65 years), when conjunctival vessels naturally thin.5
Subconjunctival Hemorrhage Recurrence Score
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
Eye-care providers diagnose the condition with a focused history and slit-lamp exam:
- Inspection: well-demarcated subconjunctival blood that stops at the limbus (cornea is clear).3
- Pupils, intraocular pressure, and vision remain normal.
- Blood pressure measurement and review of anticoagulant use help uncover systemic contributors.4
- Imaging (CT/MRI) is reserved for trauma with suspected orbital fracture or bleeding disorders.
Laboratory tests (CBC, coagulation panel) are considered when hemorrhages are recurrent, bilateral, or accompanied by easy bruising.
Treatment and Management
In most cases, reassurance is the primary therapy. The body clears the blood naturally in 7–21 days. Helpful measures include:
- Artificial tears 3–4×/day for comfort.2
- Avoidance of heavy lifting, forceful coughing, or eye-rubbing during healing.5
- Monitor blood pressure and discuss medication adjustments with a primary-care provider.
- Topical antibiotics are not required unless concomitant trauma created an open wound.6
If the bleed follows eye surgery, follow postoperative instructions; surgeons may prescribe lubricants or mild steroids to speed clearing.
Living with Subconjunctival Hemorrhage and Prevention
Because episodes can recur, building eye-healthy habits is key:
- Control systemic hypertension and diabetes with regular check-ups and medication adherence.4
- Use safety goggles for high-impact sports or dusty work environments.
- Practice sneeze and cough etiquette: exhale through partially closed lips to reduce venous spikes.5
- Limit alcohol and quit smoking, both of which impair vessel integrity.
- Stay hydrated and apply lubricating drops if you have chronic dry-eye, reducing the urge to rub.
Most people resume normal activities immediately; cosmetics can conceal redness if appearance is distressing.
Latest Research & Developments
Although usually benign, subconjunctival hemorrhage has gained attention in vascular-health studies:
- A 2022 South-Korean cohort study linked first-time hemorrhage to a small but significant increase in five-year stroke and heart-attack risk, suggesting the eye may serve as an early microvascular biomarker.7
- Ophthalmic researchers are testing ultra-widefield ocular coherence tomography-angiography to quantify subconjunctival vessel density and predict fragile zones before rupture.
- Wearable blood-pressure devices paired with smartphone alerts are being piloted to notify users when systolic spikes exceed thresholds known to precipitate ocular bleeds.
- Studies are evaluating whether long-term use of platelet-friendly antihypertensives (e.g., ACE inhibitors) reduces recurrence rates compared with beta-blockers.
Recently Published in Peer-Reviewed Journals
BMC ophthalmology
July 15, 2025
Clinical observations and outcomes of dengue-associated retinopathy at a tertiary eye hospital in Nepal.
Pradhan E, Gurung R, Shrestha S, et al.
JAMA ophthalmology
June 1, 2025
Unveiling Subconjunctival Hemorrhage in Dengue Fever-Red Alert.
Mittal R, De C
Ophthalmology
May 9, 2025
Randomized Noninferiority Trial of Direct Selective Laser Trabeculoplasty in Open-Angle Glaucoma and Ocular Hypertension: GLAUrious Study.
Gazzard G, Congdon N, Azuara-Blanco A, et al.
Next Steps
If your eye bleed is painful, affects both eyes, follows significant trauma, or recurs more than twice a year, consult a general ophthalmologist or ocular-surface specialist. They can rule out deeper injuries, clotting disorders, or masquerading lesions (e.g., conjunctival tumors).
How to schedule: Many offices accept self-referrals; urgent visits are recommended for trauma or visual changes. If wait-times are long, you can connect through Kerbside for rapid tele-triage, secure messaging, and guidance on whether in-person care or blood-work is needed.
Trusted Providers for Subconjunctival Hemorrhage

Dr. Connie Wu
Specialty
Glaucoma
Education
The Warren Alpert Medical School of Brown University

Dr. Dane Slentz
Specialty
Oculoplastics
Education
Oculoplastics

Dr. Emily Eton
Specialty
Retina/Vitreous
Education
Harvard Medical School

Dr. Emily Schehlein
Specialty
Glaucoma
Education
Glaucoma

Dr. Grayson Armstrong
Specialty
Retina/Vitreous
Education
Ophthalmology

Dr. Jose Davila
Specialty
Retina/Vitreous
Education
Retina/Vitreous Surgery

Dr. Karen Chen
Specialty
Glaucoma
Education
Glaucoma

Dr. Levi Kanu
Specialty
Cornea and External Disease
Education
Cornea and External Disease

Dr. Nicholas Carducci
Specialty
Retina/Vitreous
Education
University of Pennsylvania Perelman School of Medicine