Shingles in the Eye
Also known as Herpes Zoster Ophthalmicus
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.



Overview
Shingles in the eye—called herpes zoster ophthalmicus (HZO)—occurs when the varicella-zoster virus that caused childhood chickenpox re-awakens in the ophthalmic (V1) branch of the trigeminal nerve. The result is a painful, blistering skin rash that can inflame almost every layer of the eye, from conjunctiva and cornea to retina and optic nerve. About 10–25 % of all shingles cases involve the eye, and half of untreated patients develop sight-threatening complications such as scarring keratitis, uveitis, or glaucoma.1 The risk rises sharply after age 50 because virus-specific cellular immunity wanes; each year HZO affects roughly 110 000 Americans.2 Encouragingly, early antiviral therapy and recombinant shingles vaccination have cut both incidence and severity, and new research shows that low-dose, year-long valacyclovir further reduces recurrences and post-herpetic pain.3
Symptoms
- Prodrome: one-sided burning, tingling, or stabbing scalp pain 1–3 days before any rash.4
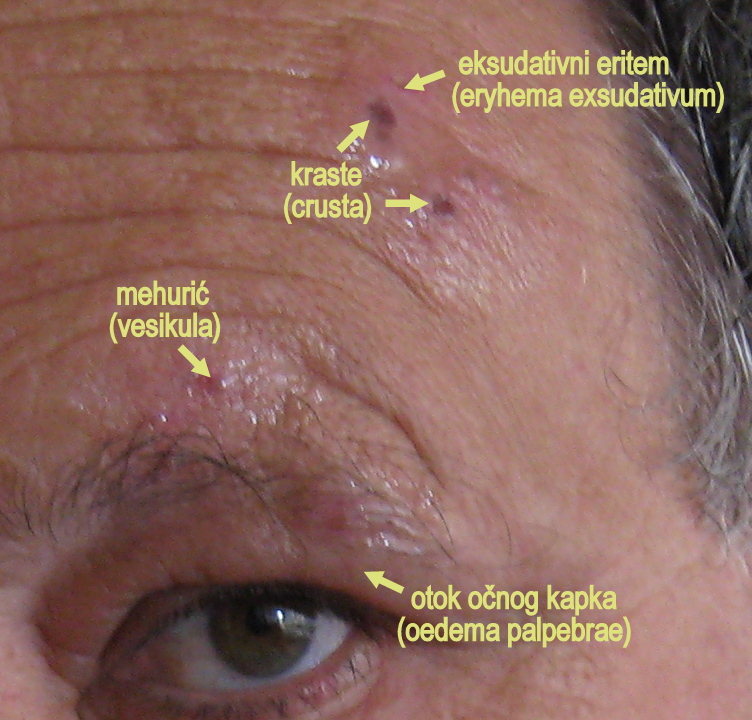
- Dermatomal rash: clusters of clear vesicles that crust on the forehead, eyelid, and often the nose tip (Hutchinson’s sign).
- Red, watery eye with photophobia and blurred vision due to conjunctivitis or keratitis.
- Light flashes or “floaters” when deeper tissues (uvea, retina) inflame.
- Neuralgia: deep aching or electric-shock pain that can linger for months.
HZO can masquerade as simple “pink eye,” so any shingles rash above the eyebrow or new eye pain after facial shingles warrants an emergency eye exam.5
Causes and Risk Factors
The virus remains dormant in cranial-nerve ganglia after chickenpox and reactivates when cell-mediated immunity drops. Major risk factors include:
- Age > 50 years—risk doubles each decade.6
- Immunosuppression from cancer therapy, HIV, organ transplant, or long-term steroids.
- Stress or severe illness that transiently lowers immune surveillance.
- Female sex and White ethnicity, which large U.S. insurance-claims studies link with higher HZO incidence.7
- Unvaccinated status; the recombinant Shingrix® vaccine lowers risk by >90 %.
30-Day Vision-Threatening Complication Risk in HZO
Select your details to estimate risk factors.
Diagnosis
- Clinical exam: a dermatomal forehead rash plus ocular findings such as pseudodendrites, keratitis, or anterior uveitis confirm HZO.8
- Slit-lamp biomicroscopy with fluorescein staining to document corneal lesions and measure intra-ocular pressure.
- Polymerase-chain-reaction (PCR) swab of a vesicle—or aqueous/vitreous tap—if the clinical picture is atypical.
- Optical coherence tomography (OCT) or ultrasound when posterior-segment inflammation or optic-nerve edema is suspected.9
Treatment and Management
Start high-dose oral antivirals within 72 hours: valacyclovir 1 g three times daily, famciclovir 500 mg three times daily, or acyclovir 800 mg five times daily for 7–10 days.10
- Topical corticosteroid drops (e.g., prednisolone 1 %) and cycloplegics control stromal keratitis or iritis—always under specialist guidance.
- Oral prednisone (40–60 mg taper) may reduce acute pain and swelling when vision is threatened.
- Analgesia: NSAIDs, gabapentin, or short-course opioids for severe neuralgia.
- Extended prophylaxis: the Zoster Eye Disease Study showed that valacyclovir 500 mg daily for one year cuts new or worsening eye inflammation by 26 % and shortens pain duration.11
Living with Shingles in the Eye and Prevention
Most patients recover good vision, but dryness, light sensitivity, or nerve pain can persist. Helpful strategies include:
- Preservative-free artificial tears and home humidifiers to calm the ocular surface.
- UV-blocking sunglasses to reduce glare and photophobia.
- Cool compresses and gentle lid hygiene to ease skin irritation.
- Vaccination: two doses of recombinant Shingrix® lower future shingles and HZO risk by >90 %.12
- Regular follow-up: every one to three months the first year to detect late-onset glaucoma or neurotrophic keratopathy.13
Latest Research & Developments
- Low-dose valacyclovir maintenance cut recurrent keratitis and iritis by 26 % in the 2024 ZEDS multicenter trial, prompting guideline reviews.14
- AAO 2024 data confirmed these benefits and highlighted reduced neuropathic-pain medication use.15
- mRNA-based VZV vaccines are entering phase-1 trials, aiming for longer-lasting immunity with fewer local reactions.
- Lipid-nanoparticle topical antivirals are being tested to deliver high corneal drug levels with minimal systemic exposure.
- AI-enabled slit-lamp imaging is under validation to grade pseudodendrites and predict who will need chronic therapy.
Recent Peer-Reviewed Research
Incidence of Giant Cell Arteritis Following Herpes Zoster Ophthalmicus: A Multicenter Retrospective Cohort Study.
Nitzan I, Shemesh N, Kubovsky S, et al.
Low-Dose Valacyclovir for Postherpetic Neuralgia in the Zoster Eye Disease Study: A Randomized Clinical Trial.
Warner DB, Jeng BH, Kim J, et al.
Acute retinal necrosis following cataract surgery: a case of VZV reactivation and successful management.
Luo T, Wang L, Zhang L, et al.
Next Steps – See an Eye Specialist Quickly
Who to see: Arrange an urgent visit with a cornea or uveitis specialist if you develop shingles on your forehead, eye redness, or vision changes. Early therapy is crucial to prevent scarring and glaucoma.
How to schedule: Ask your primary-care doctor to mark the referral “herpes zoster ophthalmicus – evaluate within 24 hours.” Many eye centers reserve same-day slots. Tele-triage nurses can coordinate imaging and courier antivirals to your pharmacy before the appointment.16 You can also connect directly with board-certified ophthalmologists on Kerbside for a medical-education consult (no patient-physician relationship will be established) to review treatment timing, insurance questions, and vaccine eligibility.17
Trusted Specialists
Board-certified providers specializing in Shingles in the Eye.
