Eye Discharge
Also known as Eye Mucus, Goopy Eyes
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
Eye discharge (sometimes called eye mucus, eye gunk, or "sleep" in your eyes) is a mix of tears, oils, skin cells, and debris that your eyes naturally wash away. A little crust in the morning is normal. But discharge that is thick, colored, foul-smelling, or keeps coming back can signal irritation or infection and deserves attention. 1
Common causes include pink eye (conjunctivitis), blepharitis (eyelid inflammation), dry eye, contact lens problems, and blocked tear ducts. When the discharge is heavy or pus-like, it may point to infection and you should be checked by an eye professional. 2
Symptoms
Symptoms vary with the cause. You might notice:
- Watery, stringy, or thick discharge that can be clear, white, yellow, or green. Lashes may crust or stick together, especially after sleep. 3
- Redness and irritation of the white of the eye and inner eyelids, sometimes with itching or a gritty feeling.
- Light sensitivity or blurred vision when discharge coats the surface of the eye.
- Both eyes involved (often allergies or viral pink eye) versus just one eye at first (sometimes bacterial or blocked tear duct).
Get same-day care if you wear contact lenses, have eye pain, or notice vision changes; these can signal a corneal infection. Pink eye can be contagious, so use good handwashing and avoid sharing towels or makeup. 4
Causes and Risk Factors
Common causes include:
- Conjunctivitis (pink eye): viral infections often cause watery discharge; bacterial infections tend to cause thicker, yellow/green discharge.
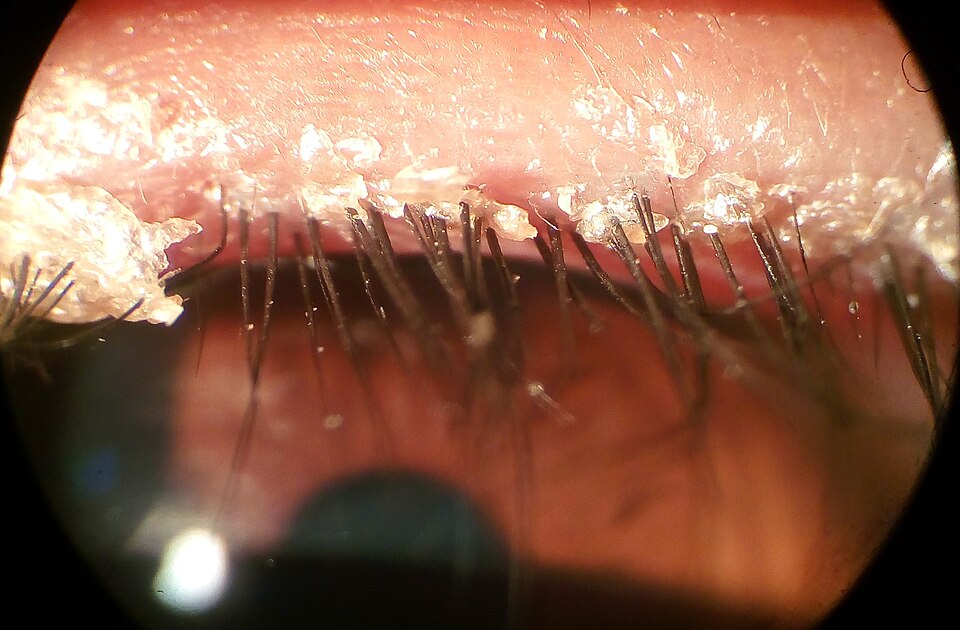
- Blepharitis: inflammation of the eyelid edges with crusting on the lashes and recurring discharge. 5
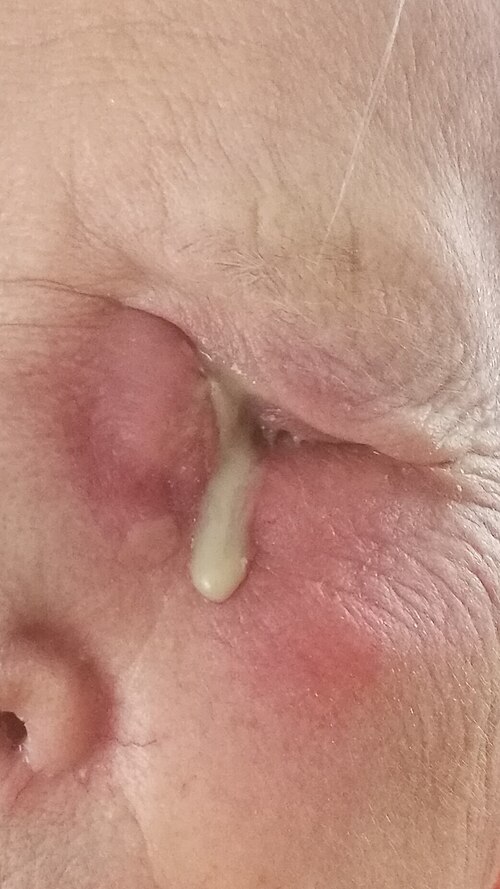
- Blocked tear duct / dacryocystitis: poor tear drainage causing tearing and sometimes pus at the inner corner. 6
- Allergies and irritants: pollen, smoke, or chemicals can trigger itchy, watery discharge.
- Contact lens issues: overwear, poor hygiene, or sleeping in lenses increases infection risk.
Higher risk: contact lens users, school-aged children, people with eyelid/skin conditions (dandruff, rosacea), and newborns.
Eye Discharge Triage Score (EDTS)
Select your details to estimate risk factors.
Diagnosis
Eye doctors diagnose the cause by examining the eyes and lids and reviewing symptoms and lens use. They may:
- Check the conjunctiva and cornea with a light and dye for scratches, ulcers, or contact lens–related problems.
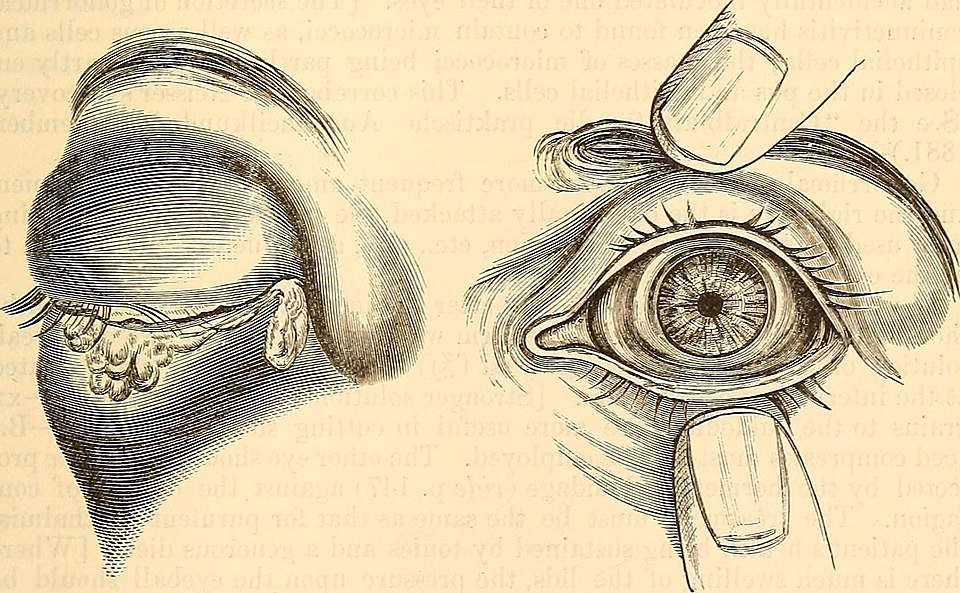
- Examine the eyelid edges and lashes for crusting, oil gland blockage, or mites.
- Press gently at the inner corner to see if pus comes from a blocked tear sac.
- Occasionally swab/culture discharge when symptoms are severe, persistent, or unusual—because appearance alone is not specific for bacterial infection. 7
Most pink eye is diagnosed by exam and history without special tests. 8
Treatment and Management
Treatment depends on the cause. In all cases: wash hands often, avoid rubbing, and stop contact lenses until an eye professional says it’s safe.
- Viral conjunctivitis: usually improves on its own; use cool compresses and artificial tears. Most OTC "redness" drops don’t speed healing. 9
- Bacterial conjunctivitis: antibiotic drops/ointment may be prescribed with thick pus or significant redness; delayed prescriptions can be reasonable to reduce resistance. 10
- Allergic conjunctivitis: cold compresses, preservative-free tears, and allergy drops (antihistamine/mast-cell stabilizers).
- Blepharitis: daily warm compresses and gentle lid scrubs; sometimes antibiotic or anti-inflammatory ointment.
- Blocked tear duct / dacryocystitis: warm compresses and massage for blockage; antibiotics and sometimes a procedure for infection.
Seek urgent care the same day if you have eye pain, light sensitivity, vision changes, contact lens–related redness/pain, swelling at the inner corner, or fever.
Living with Eye Discharge and Prevention
Helpful steps:
- Hygiene: wash hands often; don’t share towels, washcloths, pillowcases, or eye makeup; discard used tissues and contaminated cosmetics. 11
- Clean lids safely: warm compresses and diluted baby shampoo or lid wipes as recommended.
- Contact lenses: don’t wear while eyes are red or producing discharge; clean/replace lenses and cases as directed.
- Return to school/work: follow clinician guidance; many can return once improving and able to avoid close contact (policies vary). 12
Most cases clear in 1–2 weeks. If symptoms last longer or recur, an eye professional can evaluate for blepharitis, dry eye, or a blocked tear duct.
Latest Research & Developments
Evidence is refining when tests and antibiotics are helpful. A large surveillance study found that purulent discharge alone is not very specific for bacterial conjunctivitis, supporting careful diagnosis and antibiotic stewardship. 13 For newborns, national experts recommend routine eye prophylaxis against gonococcal infection to prevent vision-threatening neonatal conjunctivitis. 14
Recent Peer-Reviewed Research
A ductule dacryolith misdiagnosed as refractory conjunctivitis: a case report.
Li S, Huang Y, Zhang Y, et al.
Risk factors for the development of acute dacryocystitis in adults.
Demeuleneere A, Kusmierczyk J, Mombaerts I
International corneal and ocular surface disease dataset for electronic health records.
Ting DSJ, Kaye S, Rauz S, et al.
Next Steps
Who to see: comprehensive ophthalmologist or cornea/external disease specialist; optometrists can evaluate many causes and coordinate care.
How to schedule: if you have pain, light sensitivity, vision changes, contact lens–related symptoms, swelling at the inner corner, or fever, ask for a same-day urgent visit; otherwise schedule the next available and mention symptoms.
Referrals & follow-up: primary care clinicians/pediatricians can expedite referrals, especially for children/infants. Use drops/ointments exactly as prescribed and keep all follow-ups.
You can also connect with a specialist on Kerbside for a medical education consult (this does not establish a patient–physician relationship). For safety, avoid non–evidence-based home remedies (e.g., vinegar or breast milk). See common pink-eye myths and safer choices: 15