Dacryocystitis
Also known as Tear Duct Infection
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.
Overview
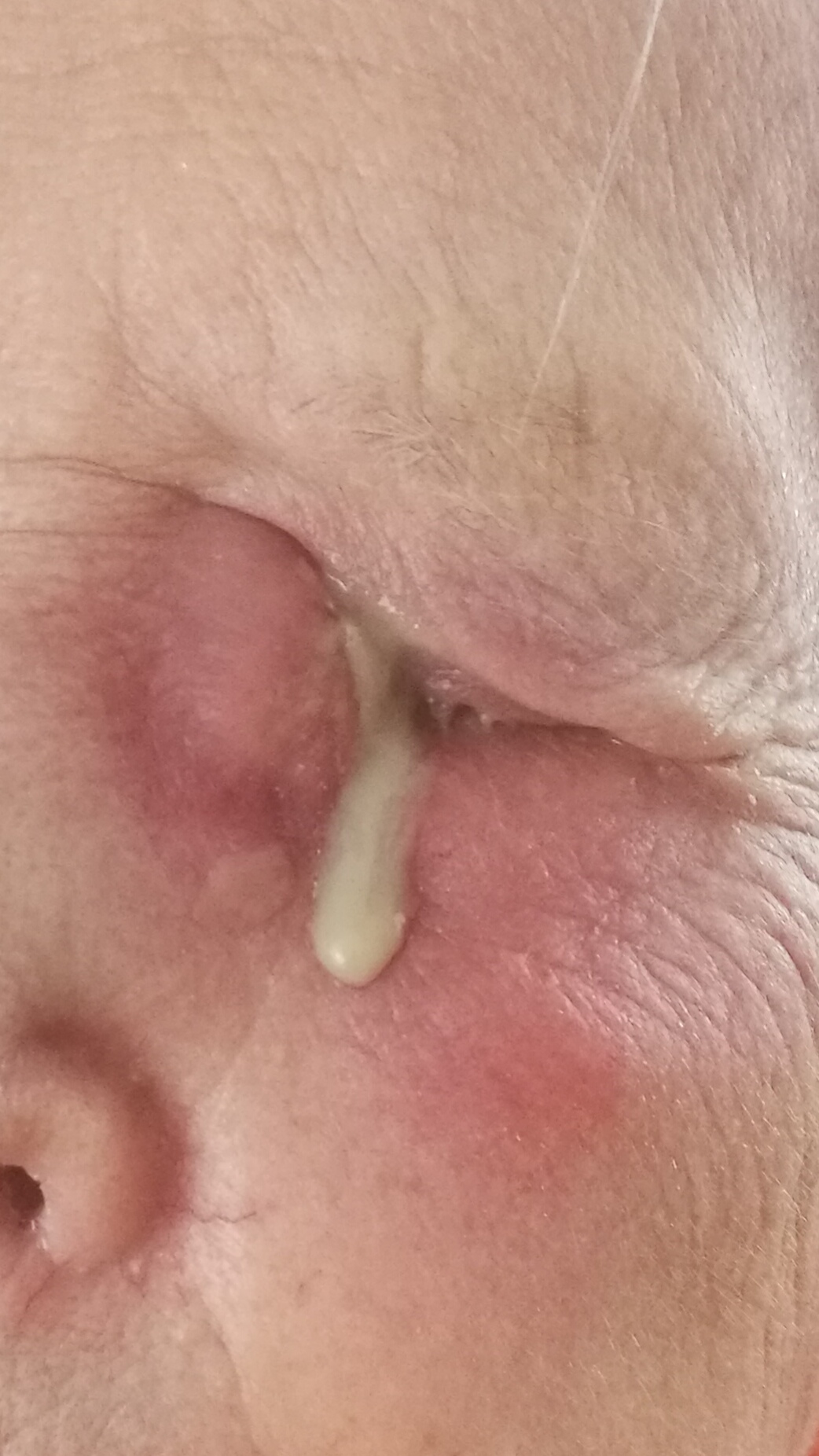
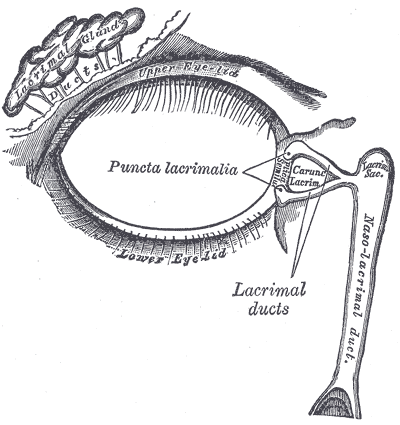
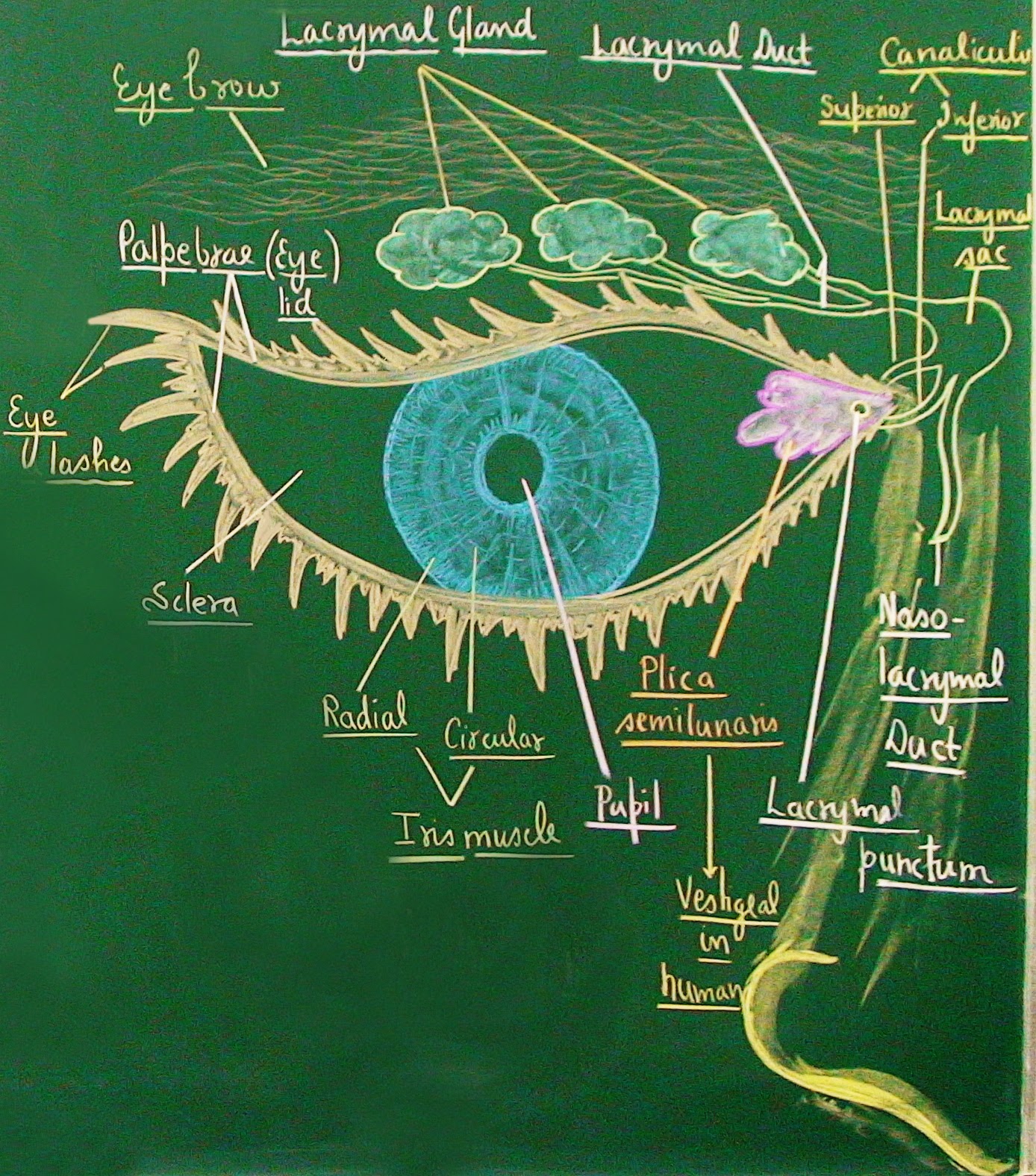
Dacryocystitis is an infection and inflammation of the lacrimal (tear) sac, the small reservoir at the inner corner of your eyelids that drains tears into the nose. It usually happens when the tear duct below the sac is blocked, causing tears and germs to pool. The area becomes red, swollen, and tender, and may drain pus. Dacryocystitis can occur at any age—newborns with tear duct blockage and adults with narrowed ducts are most commonly affected. With the right care, it is typically very treatable, but it can spread to nearby tissues if ignored. 1 2
Symptoms
Symptoms often start suddenly and are usually on one side:
- Pain, redness, and swelling near the inner corner of the eyelids (medial canthus).
- Warmth and tenderness over the lacrimal sac.
- Excess tearing, crusting, or pus from the inner corner.
- Blurry vision from tearing (vision loss is uncommon and is a red flag).
- Fever or feeling unwell in more severe cases.
In babies, signs include constant tearing from one eye, yellow-green discharge, and sometimes a bluish bump called a dacryocystocele at the inner corner. Call your clinician urgently for any of the following: spreading redness, pain with eye movement, double vision, bulging eye, high fever, or your child appearing ill—these can signal deeper infection needing emergency care. 1 2
Causes and Risk Factors
The root problem is tear duct blockage (nasolacrimal duct obstruction), which allows bacteria to multiply in a stagnant lacrimal sac. In newborns, the end of the duct may remain sealed after birth; most cases improve with growth and gentle massage. In adults, the duct can narrow or scar from age-related changes, sinus disease, nasal injury or surgery, inflammation, stones (dacryoliths), or rarely tumors. Common germs include skin and respiratory bacteria.
- Age: Newborns (congenital blockage) and adults ≥40 are most affected.
- ENT factors: Chronic sinusitis, nasal trauma, prior nasal/eye surgery.
- Other risks: Female sex, facial fractures, chronic inflammation.
Anything that blocks tear outflow can set up dacryocystitis; treating the blockage helps prevent recurrences. 2 5
Dacryocystitis Urgency & Recurrence Risk Estimator
Select your details to estimate risk factors.
Diagnosis
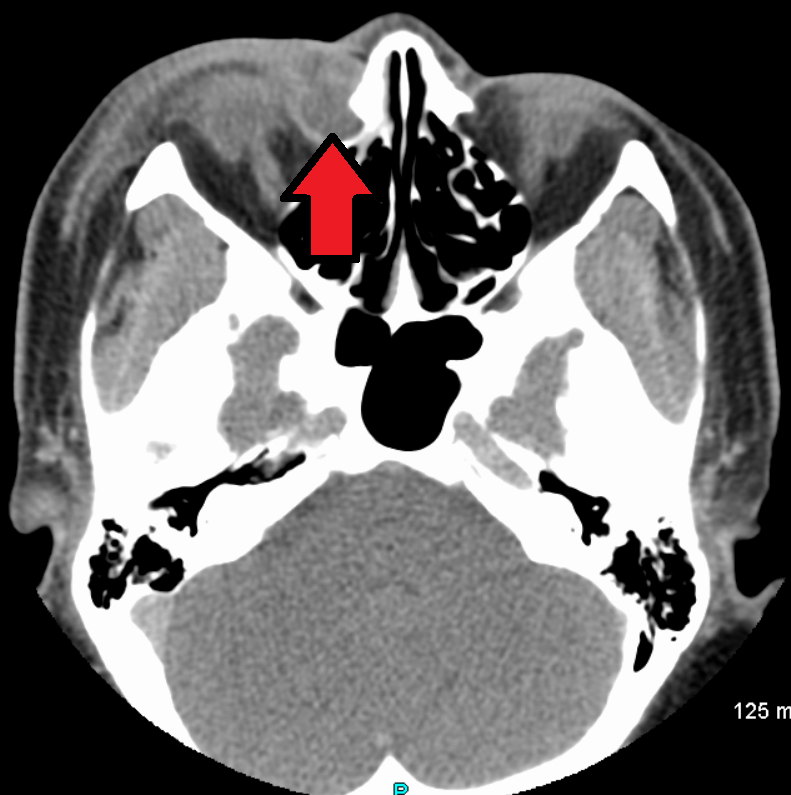
Clinicians usually diagnose dacryocystitis by history and a careful eye exam. Pressing gently over the swollen area may express pus from the tear puncta. Your provider may swab any drainage for culture if the infection is severe or unusual. If the eyelids are very swollen or there are red flags (fever, vision changes, pain with eye movement), imaging—often a CT scan—helps check for an abscess or spread to deeper tissues (preseptal/orbital cellulitis). An ophthalmologist will also look for the underlying tear duct blockage so the right long-term fix can be planned. 1 4
Treatment and Management
Goals: treat the infection now and address the tear duct blockage to prevent it from coming back.
- Immediate care (often same day): warm compresses 3–4 times daily; pain relief; antibiotics—oral for most adults and older children; IV antibiotics for infants, toxic-appearing patients, or when tissue infection is spreading. Do not squeeze or try to drain the area yourself. Contact lenses should be avoided until the infection clears.
- Drainage: if an abscess forms, a clinician may perform a small incision and drainage under sterile conditions.
- Fixing the blockage: after the acute infection settles, persistent or recurrent cases are treated by creating a new drainage path from the sac to the nose—dacryocystorhinostomy (DCR). This can be done externally (tiny skin incision) or endoscopically through the nose. Both have high success rates (roughly 85–99% for external and 91–96% for endonasal in experienced hands) and are chosen based on anatomy and surgeon expertise. 3
- Babies: most improve with time and the Crigler lacrimal sac massage taught by a clinician; short courses of antibiotic drops/ointment may be used for discharge. If blockage persists or infections recur, office probing is considered, usually after several months of age. 5
Your ophthalmologist will tailor antibiotics and procedures based on your age, severity, and exam findings.
Living with Dacryocystitis and Prevention
Most people recover fully. These steps lower the chance of recurrence:
- Use warm compresses as advised and finish any antibiotics exactly as prescribed.
- Keep eyelids clean (gentle lid hygiene) and wash hands often, especially when caring for a child with discharge.
- Treat nasal allergies or sinus problems that can worsen tear drainage.
- Avoid squeezing the swollen area; this can push infection deeper.
- Follow up to confirm the tear duct is draining and to discuss DCR if blockages keep causing infections.
Parents: if your baby’s eye is tearing, your clinician can demonstrate safe lacrimal sac massage and outline when to consider probing. Most infant blockages improve over the first year. 1 5
Latest Research & Developments
Advances focus on improving tear drainage surgery and reducing recovery time. Endoscopic DCR (through the nose) avoids a skin incision and offers success rates comparable to external DCR in many centers, with faster return to normal activities. Surgeons continue to refine stents, packing, and postoperative care to maintain the new opening and limit scarring. Ongoing studies are also comparing antibiotic strategies and drainage methods in complicated infections. Ask your surgeon which approach fits your anatomy, goals, and local expertise. 3 4
Recent Peer-Reviewed Research
Idiopathic Mixed Neutrophilic Panniculitis of the Eyelid: An Unusual Finding.
Aguilar-Falomir J, Coloma González I, Aguilar López FJ, et al.
Endoscopic Dacryocystorhinostomy in a Patient With Hemi-Arrhinia.
Kelly Z, Adil E, Reshef ER
Combined External Dacryocystorhinostomy and Cosmetic Surgery.
Parikh AO, Burnstine MA
Next Steps
If you think you have dacryocystitis, seek care promptly—especially with fever, severe pain, or vision changes. The best specialist to see is an Ophthalmologist (ideally an Oculoplastics specialist). Your primary care clinician or pediatrician can start antibiotics and help with referral if needed. For scheduling: ask about urgent slots, waitlists, and cancellation lists—eye teams often reserve time for infections. Bring a list of medicines and any prior sinus or nasal surgeries. After the infection settles, discuss how to prevent recurrence, including whether a DCR makes sense in your case.
You can also connect with the right specialist on Kerbside for a medical education consult to better understand your diagnosis and options (this is for education only and does not establish a patient–physician relationship).
Trusted Specialists
Board-certified providers specializing in Dacryocystitis.
