Orbital Cellulitis
Also known as Postseptal Cellulitis
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
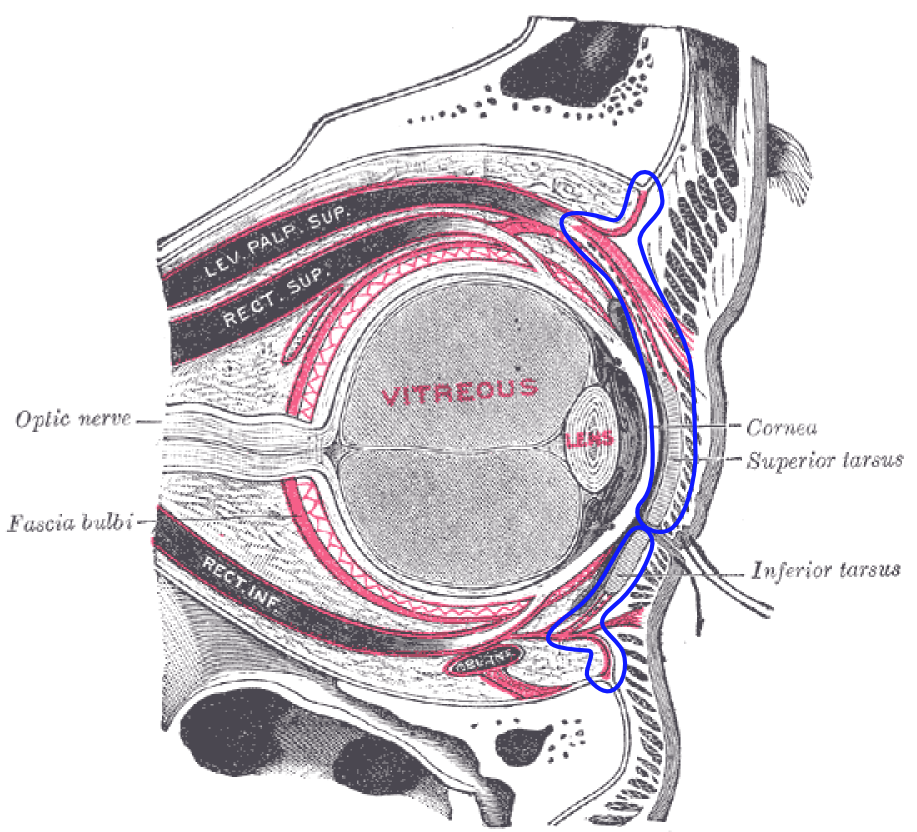
Orbital cellulitis is a serious infection of the tissues within the eye socket (orbit) that sit behind the orbital septum. It most often spreads from a nearby sinus infection and can threaten vision and, rarely, life if not treated quickly. Typical care involves urgent evaluation in the emergency department, imaging, and hospital treatment with intravenous (IV) antibiotics. Prompt treatment usually leads to a full recovery, but delays can cause permanent problems, including vision loss and brain complications. 1 2
Symptoms
Symptoms often start suddenly and can worsen over hours. Common signs include:
- Severe eyelid swelling and redness, often with fever.
- Pain with eye movement and trouble moving the eye in one or more directions (ophthalmoplegia).
- Bulging of the eye (proptosis) and double vision or blurred vision.
- Tenderness around the nose or cheeks from sinus involvement.
These findings help doctors distinguish orbital cellulitis from preseptal (periorbital) cellulitis, which affects tissues in front of the septum and usually does not cause pain with eye movement, proptosis, or limited eye movements. 3 2
Causes and Risk Factors
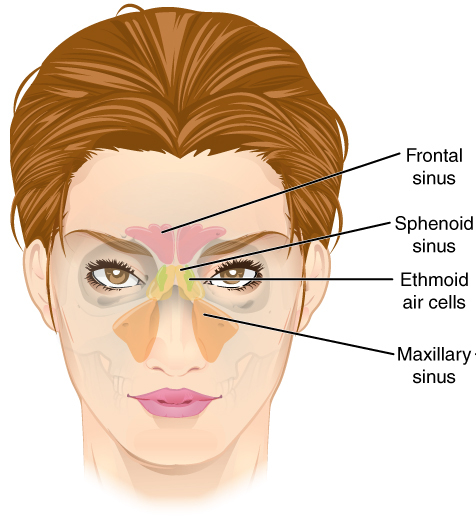
In most cases, bacteria spread into the orbit from infected paranasal sinuses, especially the ethmoid sinuses located between the eyes. Less commonly, infection enters the orbit after trauma, eye or eyelid surgery, a dental infection, or from the bloodstream. Common bacteria include Streptococcus and Staphylococcus species (including community MRSA in some areas). 1
Risk is higher in children, people with recent or ongoing sinus infections, those with diabetes or weakened immune systems, and anyone with recent facial trauma or skin infections around the eyelids or nose. 2
Orbital Cellulitis Concern Score (educational)
Select your details to estimate risk factors.
Diagnosis
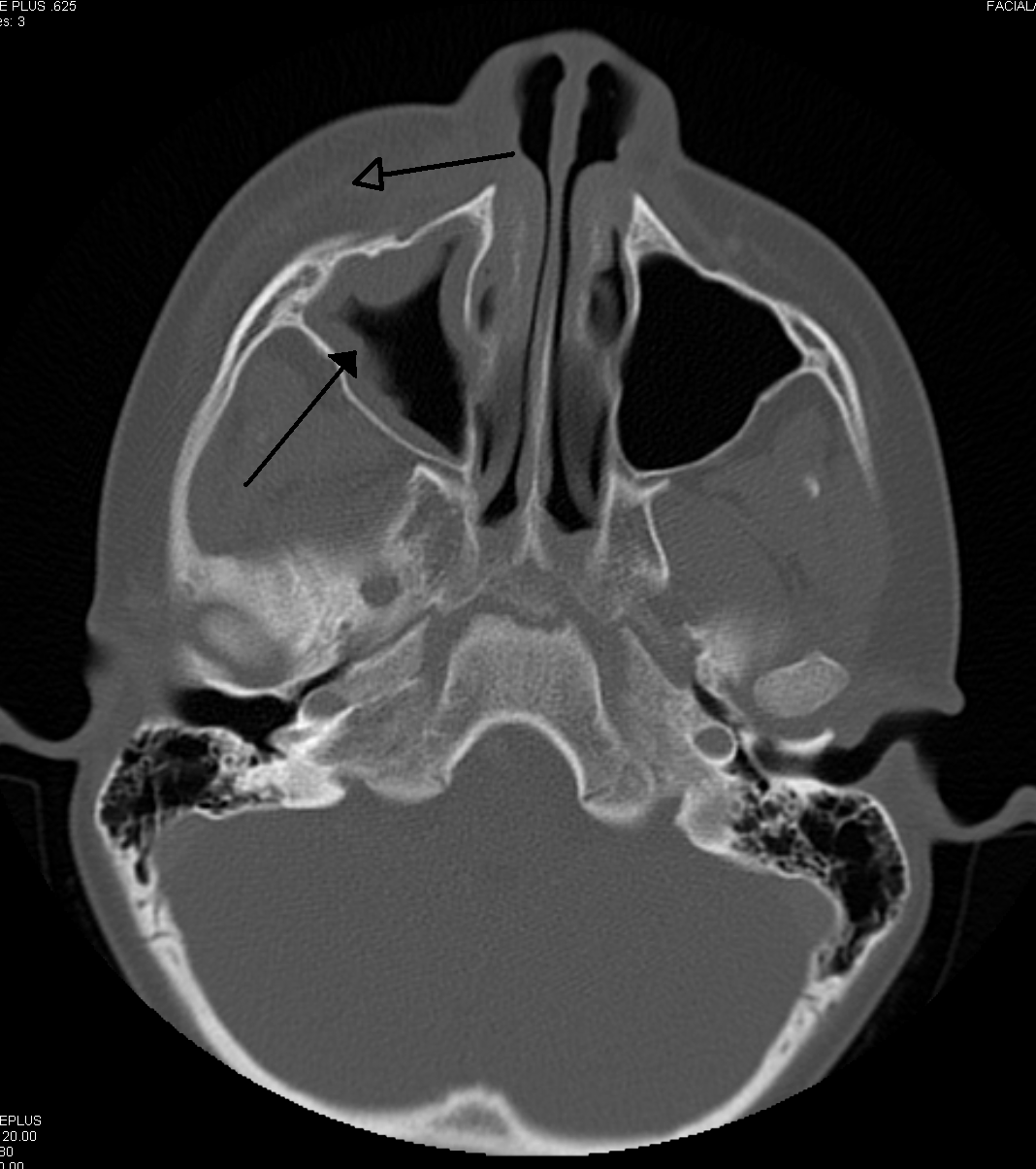
Doctors diagnose orbital cellulitis using your history, an eye exam, and imaging. Key exam findings are pain with eye movement, restricted eye movements, and proptosis. A CT scan of the orbits and sinuses is commonly used to confirm the diagnosis, look for an abscess, and guide treatment; MRI can be used when intracranial spread or cavernous sinus thrombosis is a concern. Blood tests and cultures may also be obtained. Because this condition can worsen quickly, children and most adults are evaluated urgently in the emergency department and typically admitted to the hospital for treatment and monitoring. 2 3
Treatment and Management
The mainstay of treatment is prompt IV antibiotics that cover the most likely sinus bacteria. Many hospitals start a broad regimen (for example, ampicillin–sulbactam or a third-generation cephalosporin), and add MRSA coverage (such as vancomycin) based on local patterns and clinical risk. An otolaryngologist (ENT) and ophthalmologist often co-manage care. If a subperiosteal or orbital abscess is present—or if vision is threatened, there is worsening after 24–48 hours of antibiotics, or intracranial spread is suspected—surgical drainage of the sinuses and/or orbit may be needed.
Some centers consider a short course of adjunctive steroids to reduce swelling after antibiotics are started, but evidence is limited and mixed; if used, they are started only once appropriate antibiotics are on board and under specialist guidance. 6
Living with Orbital Cellulitis and Prevention
With early treatment, most people recover well. During hospitalization, eye movements and vision are checked often. After discharge, you may take oral antibiotics to complete the course, use saline rinses if advised, and keep follow-up appointments with ophthalmology and, if needed, ENT. Call your care team right away for any return of fever, worsening eye pain, double vision, decreasing vision, or new severe headache.
Prevention focuses on treating sinus infections early, protecting the face and eyes from injury, and keeping up to date on routine vaccines (e.g., pneumococcal and Hib), which have changed the bacterial landscape of pediatric orbital cellulitis in the vaccine era. 7 1
Latest Research & Developments
Recent pediatric studies suggest that using a nasal MRSA PCR test may safely reduce unnecessary anti-MRSA antibiotics when the screen is negative, supporting more targeted therapy in selected children with orbital cellulitis. 7 Evidence on adding systemic steroids remains limited; a Cochrane review highlights uncertainty and calls for better trials to clarify if steroids shorten hospital stay or improve outcomes without increasing risk. 6
Recent Peer-Reviewed Research
A case of post-traumatic orbital cellulitis caused by Eikenella corrodens.
He N, Peng Z
Incidence of orbital cellulitis in children: a population-based study.
Vloka CN, Summers RC, DeSantis D, et al.
Clinical Stage of Retinoblastoma Based on Presenting Signs of 4578 Patients from 121 Countries.
Yanagihara RT, Takayesu JSK, Crotty EE, et al.
Next Steps
If you or your child has warning signs like fever with painful eye movements, double vision, bulging of the eye, or vision changes, seek emergency care immediately.
The most appropriate specialist to coordinate care is a board-certified ophthalmologist (ideally with oculoplastics/orbital expertise), often in collaboration with an ENT surgeon. In many regions, you may need a referral from your primary care clinician or pediatrician. If the first available appointment is far out, ask to be placed on a waitlist and request a same-day cancellation slot; for urgent symptoms, go to the emergency department rather than waiting for clinic time.
You can also connect directly with the right specialist on Kerbside for a medical education consult to understand your condition and care options. This is for education and navigation; no patient–physician relationship is established.