Burning Eyes
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.


Overview
Burning eyes is a common symptom that feels like stinging, heat, or irritation on the surface of the eye. It often comes with redness, tearing, or a gritty sensation. The most frequent causes are dry eye, eyelid inflammation (blepharitis), allergies, irritants like smoke or wind, and sometimes eye infections.
Most cases are mild, but sudden severe pain, vision changes, or chemical exposure need urgent care. An eye doctor can identify the cause and suggest simple steps that bring relief. 1
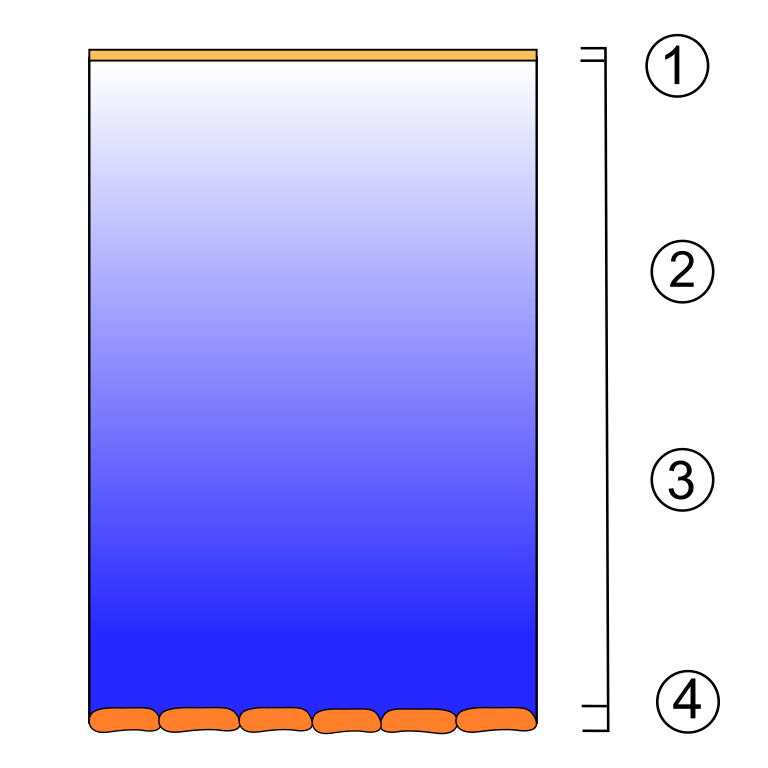
Dry eye disease is especially common and can make eyes burn because the tears don’t lubricate well or evaporate too quickly. 2
Symptoms
People describe burning eyes in many ways. You might notice:
- Stinging or a hot, scratchy feeling.
- Redness, watery eyes, or the sense that something is in your eye.
- Blurred vision that clears after blinking, and trouble with contact lenses. 4
- Itching and discharge, which can point to allergies or infection. 5
Get urgent help if you have chemical exposure, a sudden drop in vision, severe pain, or new light sensitivity. These can signal a more serious problem and should be checked the same day.
Causes and Risk Factors
Common causes include:
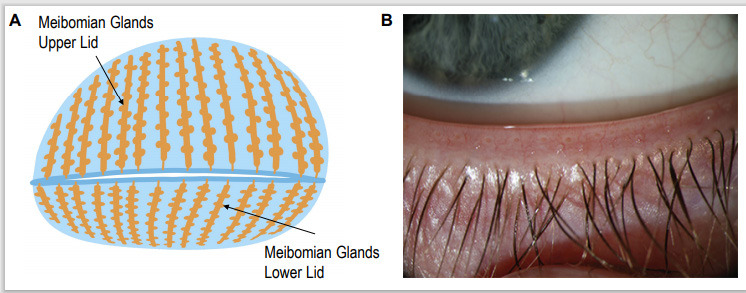
- Dry eye and meibomian gland dysfunction (MGD): When tear quality is poor or evaporates fast, the surface dries and burns. Risk factors include age, being female, certain medicines (like antihistamines), autoimmune disease, and screen time.
- Allergies (allergic conjunctivitis): Burning with itching and stringy mucus points to allergies.
- Irritants and environment: Smoke (including wildfire smoke), wind, dry indoor air, and pollution can trigger burning and tearing. 6
- Infections: Viral and bacterial conjunctivitis can burn and sting, often with discharge.
- Eye strain and digital use: Fewer blinks during screen time can worsen dryness and burning. 7
- Contact lens issues: Overwear, poor fit, or deposits can irritate the surface.
Burning Eyes Triage Score
Select your details to estimate risk factors.
Diagnosis
An eye care professional will ask about your symptoms, environment, allergies, and contact lens use, then examine your eyes with a microscope (slit lamp). To find the cause, they may perform:
- Tear film tests: Tear break-up time and Schirmer testing to measure tear quality and amount. 2
- Fluorescein staining: To look for dry spots or tiny abrasions.
- Eyelid and oil gland evaluation: For MGD/blepharitis. Swabs may be taken if infection is suspected. 3
The goal is to match treatment to the cause so your eyes feel better quickly.
Treatment and Management
Treatment depends on the cause. Many people feel better with a few targeted steps:
Quick relief at home:
- Use preservative-free artificial tears 2–6×/day; gels or ointments help at night.
- Follow the 20-20-20 rule for screens (every 20 minutes, look 20 feet away for 20 seconds) and blink fully.
- Warm compresses and gentle lid hygiene (dilute cleanser or eyelid wipes) if lids are crusty or oily—this helps MGD.
- Use a humidifier, wear wraparound sunglasses outdoors, and avoid smoke or direct air from fans/vents. 6
Medications and drops:
- Allergy drops (antihistamine/mast-cell stabilizer) for itchy, allergic burning.
- Prescription anti-inflammatory drops (such as cyclosporine or lifitegrast) for moderate–severe dry eye; a short steroid course may be used by your doctor for flares. 4
Procedures and devices:
- Punctal plugs to slow tear drainage in stubborn dryness.
- In-office eyelid heat/expression for MGD; some clinics offer intense pulsed light (IPL) as an adjunct in select patients.
Important: If a chemical gets in your eye, flush with clean water or saline for at least 15 minutes and seek emergency care right away.
Living with Burning Eyes and Prevention
Daily habits can calm burning and help prevent flare-ups:
- Manage your environment: Use a humidifier, aim car/home vents away from your face, and wear sunglasses on windy days. During wildfire smoke events, stay indoors when air quality is poor and use preservative-free tears more often.
- Screen-smart routines: Take regular breaks and blink fully to keep tears spread evenly. 7
- Lid care: If you have blepharitis or MGD, do warm compresses and gentle lid cleaning most days.
- Allergy control: Rinse eyes with preservative-free tears after outdoor exposure; consider allergy drops if your clinician recommends them. 5
- Contact lens hygiene: Follow wear time, replace on schedule, and never sleep in lenses unless approved.
Most people with burning eyes improve with simple steps and, when needed, targeted treatments from an eye professional.
Latest Research & Developments
New options are expanding care for people with burning from dry eye and MGD:
- Varenicline nasal spray: Stimulates natural tear production and has FDA approval for dry eye signs and symptoms. 9
- Intense Pulsed Light (IPL): Combined with meibomian gland expression, IPL is showing benefit in clinical trials for MGD-related dry eye. 10
Ask your eye specialist whether these or other emerging therapies are a good fit for you.
Next Steps
Who to see: Start with your primary eye-care provider. For persistent or severe burning, especially with dry eye or eyelid problems, see a cornea/external disease ophthalmologist. They can confirm the cause and offer advanced treatments.
How to schedule: When you call, mention your key symptoms (for example, burning with vision blur or contact lens pain). Ask about urgent slots, waitlists, or cancellation lists if your symptoms are getting worse. If you had a chemical exposure or sudden vision changes, seek same-day urgent or emergency care.
What to bring: A list of all drops and medicines, your contact lenses/case, and details about exposures (smoke, dust, new cosmetics), screen time, and sleep.
Kerbside option: You can also connect through Kerbside for a medical education consult with the right specialist to review your situation and next steps. This is for guidance only and does not create a patient–physician relationship.