Itchy Eyes
Also known as Ocular Pruritus
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.
Overview
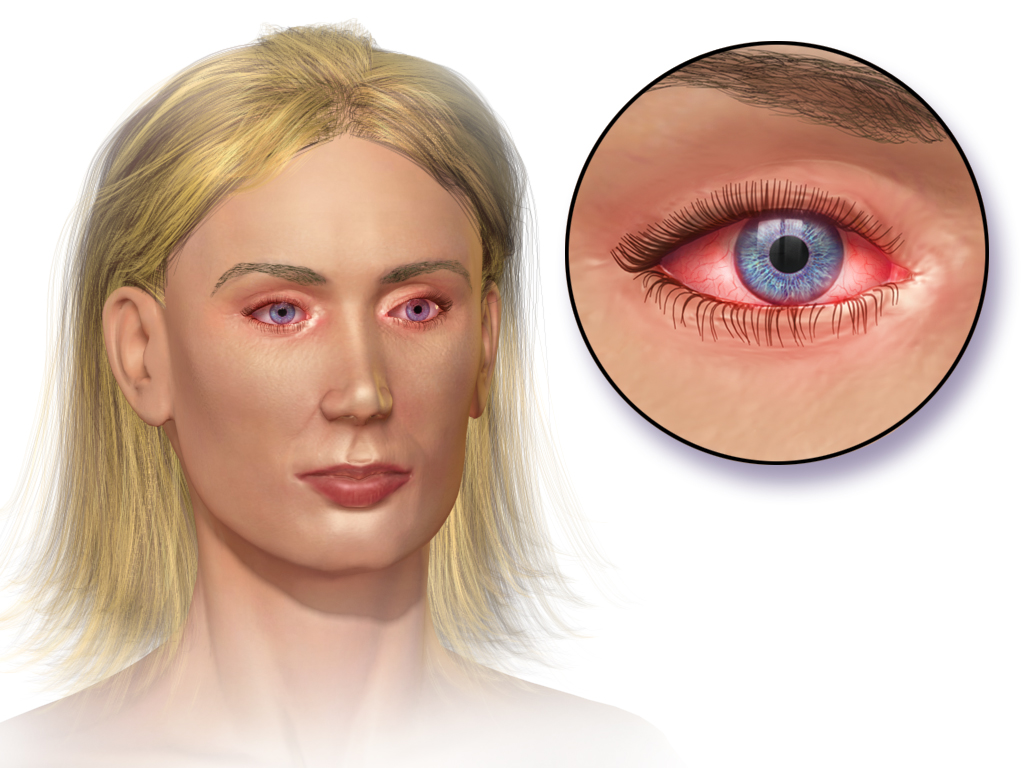
Itchy eyes are very common. Most of the time, itching happens because the clear tissue covering the white of your eye and inside of your eyelids (the conjunctiva) gets irritated or inflamed. Allergies are a frequent cause, but dryness, eyelid problems, contact lenses, and infections can also make your eyes itch.
Knowing the pattern of your symptoms and what triggers them can help you and your clinician decide what to do next. Many cases can be eased with simple steps at home, while some need an eye exam or prescription treatment.
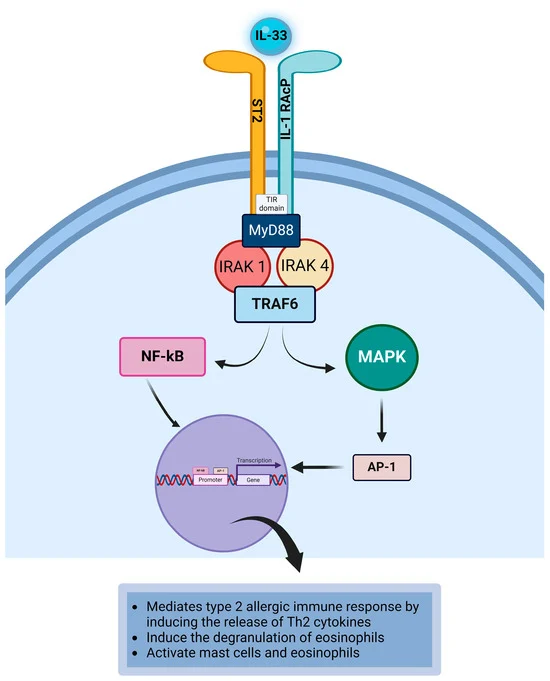
When allergies are to blame, you may also notice redness, tearing, and watery or stringy discharge. These symptoms often affect both eyes and may come with sneezing or a stuffy nose. This is called allergic conjunctivitis, and it is very treatable with avoidance, artificial tears, and allergy eye drops. 1
If you have strong pain, very light-sensitive eyes, vision changes, or thick pus, that is different and should be checked promptly because infections like “pink eye” or other conditions may be present. 2
Symptoms
People describe itchy eyes as a tickle, burning, or the urge to rub. You might have:
- Redness, tearing, or puffy eyelids
- Clear, watery or stringy discharge (often with allergies)
- Runny or itchy nose, sneezing, or scratchy throat (typical with seasonal allergies)
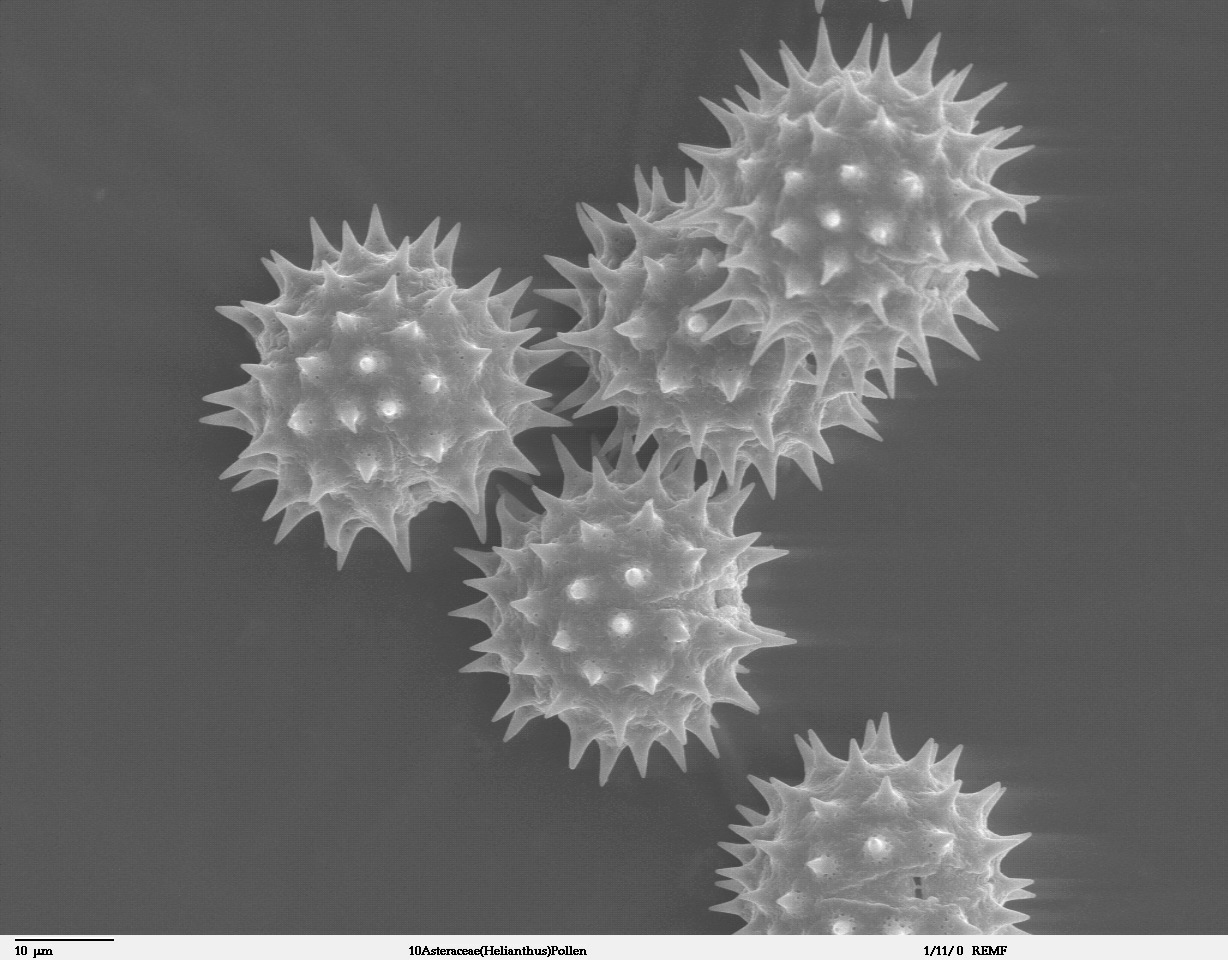
Allergy-related itching usually affects both eyes and may flare during pollen seasons or around pets, dust, or mold. 3
See a clinician right away for severe pain, very red eyes, strong light sensitivity, vision changes, thick yellow-green discharge, or if symptoms do not improve after a few days of care. These can signal an infection or another eye problem that needs treatment. 2
Causes and Risk Factors
Common causes of itchy eyes include:
- Allergic conjunctivitis (seasonal or year-round): Pollen, pet dander, dust mites, and mold are typical triggers. Less common forms include vernal and atopic keratoconjunctivitis, and contact lens–related allergy (giant papillary conjunctivitis). These often bring strong itching, tearing, and swelling in both eyes.
- Eyelid inflammation (blepharitis): Oil gland problems and bacteria at the lash line can cause itching, crusting, and irritation—often worse on waking. Gentle, regular lid hygiene helps, and sometimes medicines are needed. 4
- Dry eye and irritants: Smoke, chlorine, perfumes, and air pollution can sting and itch. Screen time and dry rooms can worsen symptoms.
- Infections: Viral or bacterial conjunctivitis may itch, but thick discharge, one-eye start, or fever favors infection. Infections spread easily, so hand washing and not sharing towels or makeup are important. 2
Risk is higher if you have seasonal allergies, asthma or eczema, wear contact lenses, have eyelid skin conditions, or are often exposed to triggers (like pollen or pet dander).
Allergic Itchy Eye Likelihood Score
Select your details to estimate risk factors.
Diagnosis
Clinicians diagnose itchy eyes by asking about your symptoms and examining your eyes and eyelids. They look at whether one or both eyes are affected, the type of discharge, and the timing (for example, every spring). A slit-lamp exam may show allergy swelling, papillae under the eyelid, or signs of dryness or blepharitis.
In hard-to-tell cases, your clinician might consider simple tests (such as eyelid/tear evaluations) or work with an allergist for skin or blood testing to find triggers. 3
If an infection is suspected, an exam usually suffices; rarely, lab tests of the discharge are needed. 2
Call urgently for severe pain, light sensitivity, sudden vision changes, or an eye injury.
Treatment and Management
Most people feel better with a mix of trigger control and the right eye drops:
- Quick comfort: Use cool compresses and preservative-free artificial tears to rinse allergens and soothe irritation.
- Allergy eye drops: Over-the-counter antihistamine/mast-cell stabilizer drops (e.g., ketotifen or olopatadine) relieve itching and redness. Combination or prescription options are available if needed.
- Oral antihistamines: Can help whole-body allergy symptoms but may dry the eyes. Choose non-drowsy types when possible and ask your clinician if they are right for you.
- Decongestant/“redness relief” drops: Avoid using longer than a couple of days because they can cause rebound redness; not for people with certain conditions like glaucoma.
- Prescription options: Short courses of steroid eye drops may be used for severe allergy under an eye specialist’s close supervision. Other options include stronger dual-action drops or, for stubborn allergies, allergen immunotherapy guided by an allergy specialist. 6
- Eyelid care: For blepharitis, daily warm compresses and gentle lid cleaning often help; your clinician may add medicines if needed. 4
- Contact lens tip: If your eyes are itchy or red, take a break from lenses, switch to glasses, and replace your case and solution. Restart lenses only after your symptoms are gone.
Living with Itchy Eyes and Prevention
Small habits make a big difference:
- Do not rub your eyes. Rubbing releases more histamine and can worsen swelling and redness.
- Rinse and shield: Use artificial tears after outdoor time; wear wraparound glasses or sunglasses on high-pollen days; keep windows closed and use air conditioning in car and home during peak pollen seasons.
- Allergen control at home: Wash pillowcases weekly in hot water, consider dust-mite covers, control indoor humidity (30–50%), and keep pets out of the bedroom if they trigger symptoms.
- Makeup & hygiene: Replace eye makeup every 3 months; never share cosmetics. Wash hands often, especially if an infection is suspected, and do not share towels or eye drops. 2
- Screen & air: Use a humidifier in dry rooms and take breaks from screens to reduce dryness.
- For frequent seasonal flares, start allergy eye drops before your bad season, and talk with your clinician about longer-term options, including immunotherapy if symptoms remain tough to control. 6
Latest Research & Developments
Research supports antihistamine and mast-cell stabilizer eye drops—alone or as dual-action formulas—as safe and effective for reducing allergic eye itching and redness. 7
Newer once-daily options and preservative-free tears can improve comfort and make it easier to stick with treatment.
For people with severe or year-round disease, clinicians may combine drops with short, carefully monitored steroid courses or consider allergy shots (immunotherapy) when appropriate. Immunotherapy targets the root cause by training your immune system to react less to triggers, and it may help when medicines alone are not enough. 6
There is also growing attention on eyelid and tear-film health (like treating blepharitis and dryness), contact lens strategies (daily disposables, proper hygiene), and environmental controls to reduce exposure—practical steps that can lower flares while you continue daily life.
Recent Peer-Reviewed Research
Prominent corneal nerves in pure mucosal neuroma syndrome, a clinical phenotype distinct from multiple endocrine neoplasia type 2B.
Yin L, Wang Y, Zhu J, et al.
[CLINICAL EFFICACY OF SUBLINGUAL IMMUNOTHERAPY WITH CEDAR POLLEN IN A YEAR OF MASSIVE CEDAR POLLEN DISPERSAL AND ITS EFFECT ON JAPANESE CYPRESS POLLINOSIS].
Yuta A, Ogawa Y, Kozaki H, et al.
[ENHANCED CLINICAL EFFECTS OF CEDARCURE(®) TABLETS OF SUBLINGUAL IMMUNOTHERAPY OVER THE YEARS OF TREATMENT AND THE IMPACT OF OUTCOME BY COMBINED USE OF MITE SUBLINGUAL IMMUNOTHERAPY (DUAL SLIT) FOR JAPANESE CEDAR POLLINOSIS].
Yuta A, Ogawa Y, Murao T, et al.
Next Steps
If your itchy eyes are mild, start with cool compresses and preservative-free artificial tears. If symptoms last more than a few days, keep coming back, or include strong pain, light sensitivity, blurred vision, or thick discharge, arrange a visit.
Best specialist to see: Ophthalmologist (Cornea/External Disease). They can check for allergy, dry eye, blepharitis, contact lens problems, and infections, and then tailor safe treatment. An Allergist/Immunologist is helpful if your symptoms are frequent, tied to clear triggers (like pollen or pets), or you are considering allergy testing or shots.
How to schedule:
- Call your primary care clinician or eye doctor for the soonest appointment; ask about urgent slots if you have warning signs.
- Join the clinic’s cancellation/wait list and check for same-day openings. Ask if photos or a brief triage call can speed care.
- Bring your current drops, allergy meds, and contact lenses/case to your visit. Pause contact lens wear until cleared.
- Check your insurance for referral needs before booking, especially for specialty clinics.
You can also connect directly with the right specialist on Kerbside for a medical education consult to understand your options and next steps (this does not establish a patient–physician relationship).