Contact Lens Keratitis
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.
Overview
Contact lens keratitis is an infection or severe inflammation of the cornea (the clear front window of the eye) that occurs more often in contact lens wearers. Germs such as Pseudomonas bacteria, fungi, or the parasite Acanthamoeba can enter tiny surface breaks and cause a painful sore (ulcer). Sleeping in lenses, water exposure, and poor cleaning raise the risk. 1
Keratitis can threaten vision if not treated quickly, but most cases improve with fast care and proper medicine. Regular eye exams and healthy lens care are key to prevention. 2
Symptoms
Symptoms can develop quickly (hours to days) and may include:
- Eye pain or soreness (moderate to severe)
- Redness and tearing
- Light sensitivity (photophobia)
- Blurry vision or a white/gray spot on the cornea
- Discharge and trouble wearing the lens
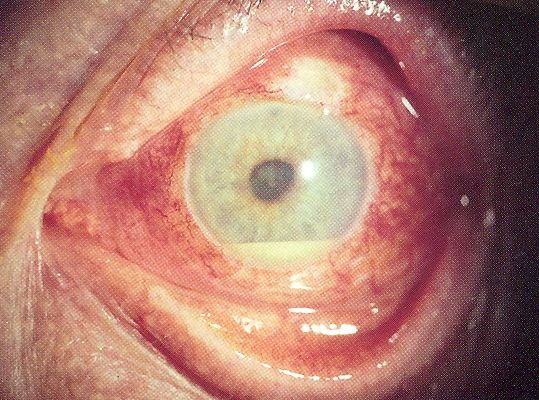
Sometimes a layer of white cells settles in the front of the eye (hypopyon), showing strong inflammation. Remove lenses and seek urgent same-day care if these occur. 3
Causes and Risk Factors
Keratitis happens when germs reach and invade the cornea. In lens wearers, risk rises if the surface is stressed or the lens/case carries microbes. Major risks include:
- Sleeping or napping in lenses (especially extended-wear types)
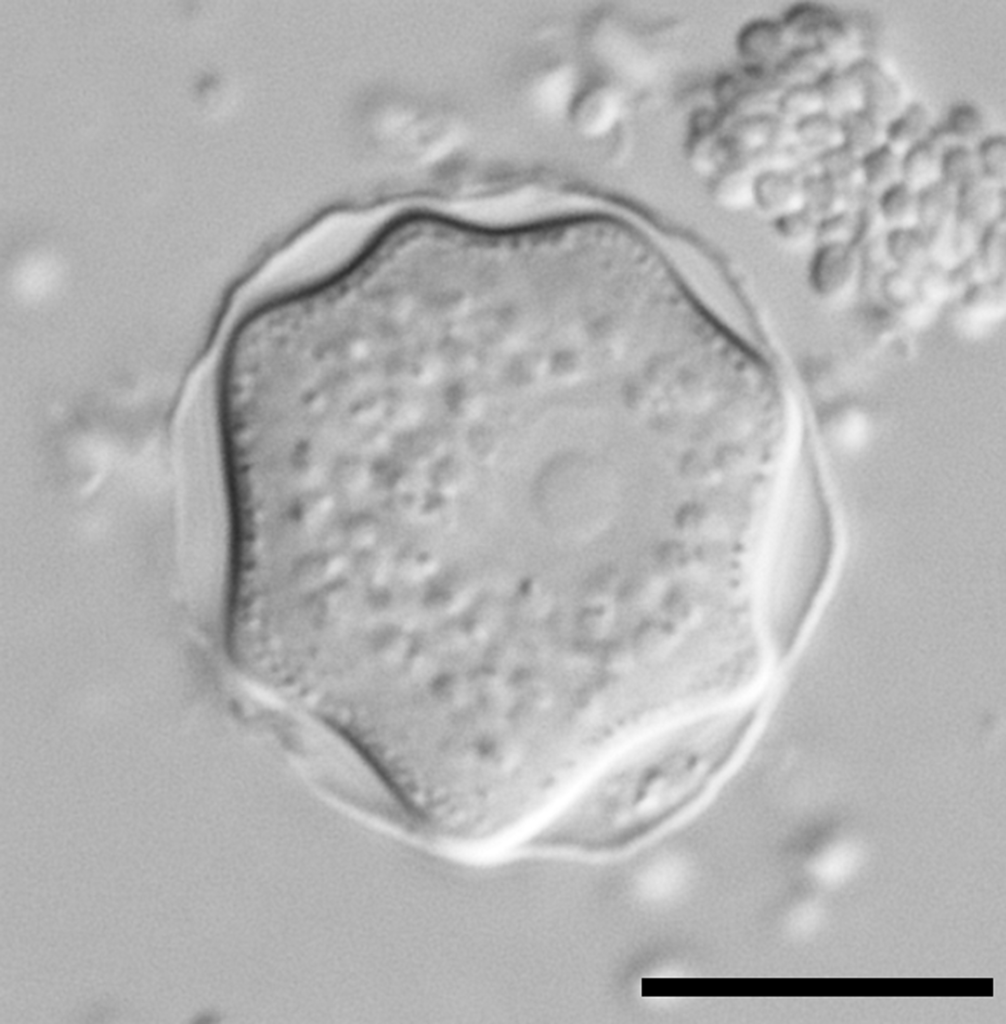
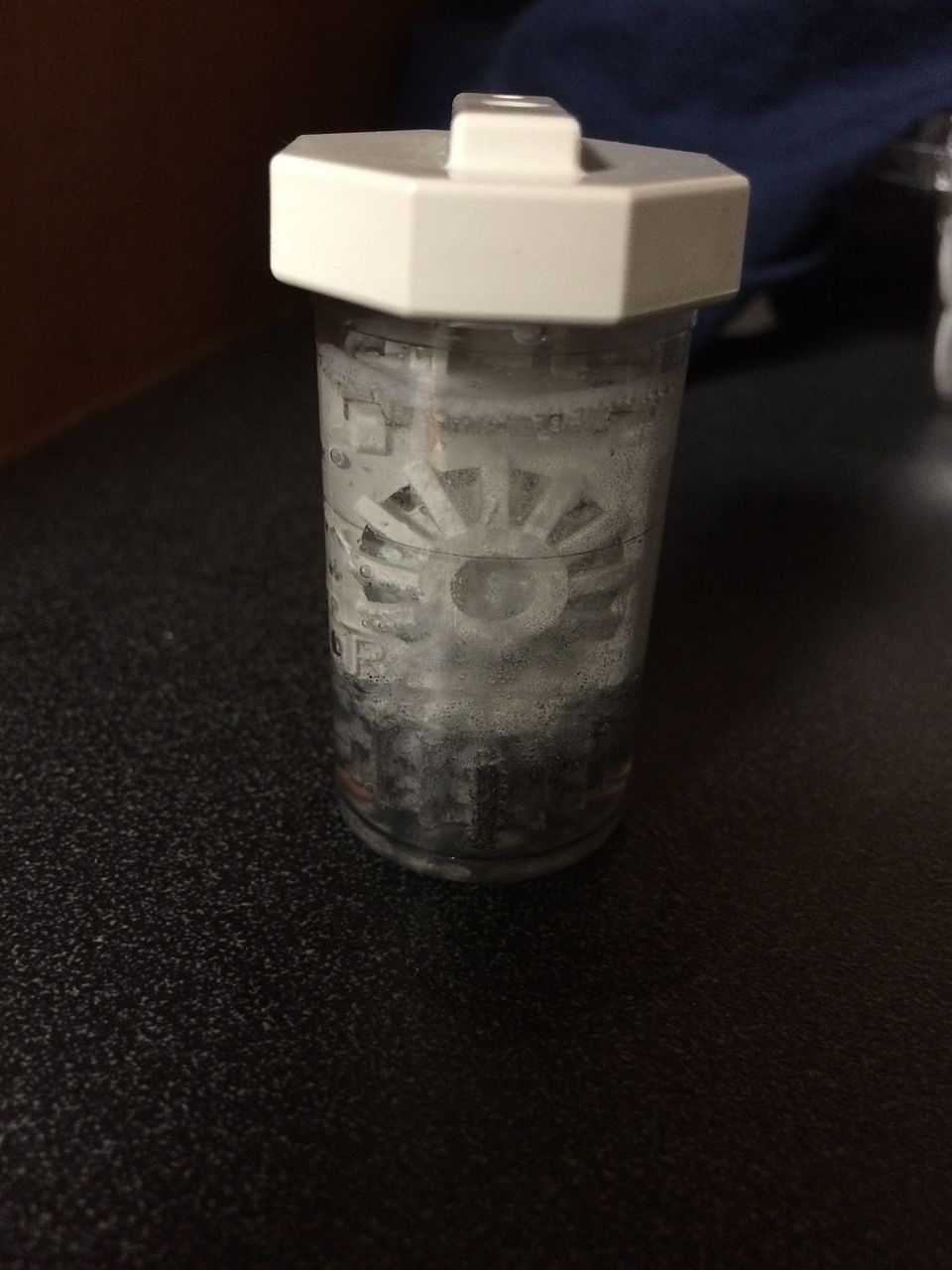
- Water exposure: swimming, showering, or rinsing lenses/cases with tap water (raises Acanthamoeba and other risks)
- Poor hand hygiene, topping off old solution, or skipping the rub-and-rinse step
- Over-wearing lenses, stretching replacement, or not replacing the case every 3 months
- Eye trauma or dry eye that weakens the surface
Lens wear increases risk for bacterial keratitis when lenses are worn too long or cared for incorrectly, and water exposure is a well-known risk for Acanthamoeba. 4 5
Contact Lens Keratitis: Simple 1-Year Risk from Wear & Care Habits (Assumption-Based)
Select your details to estimate risk factors.
Diagnosis
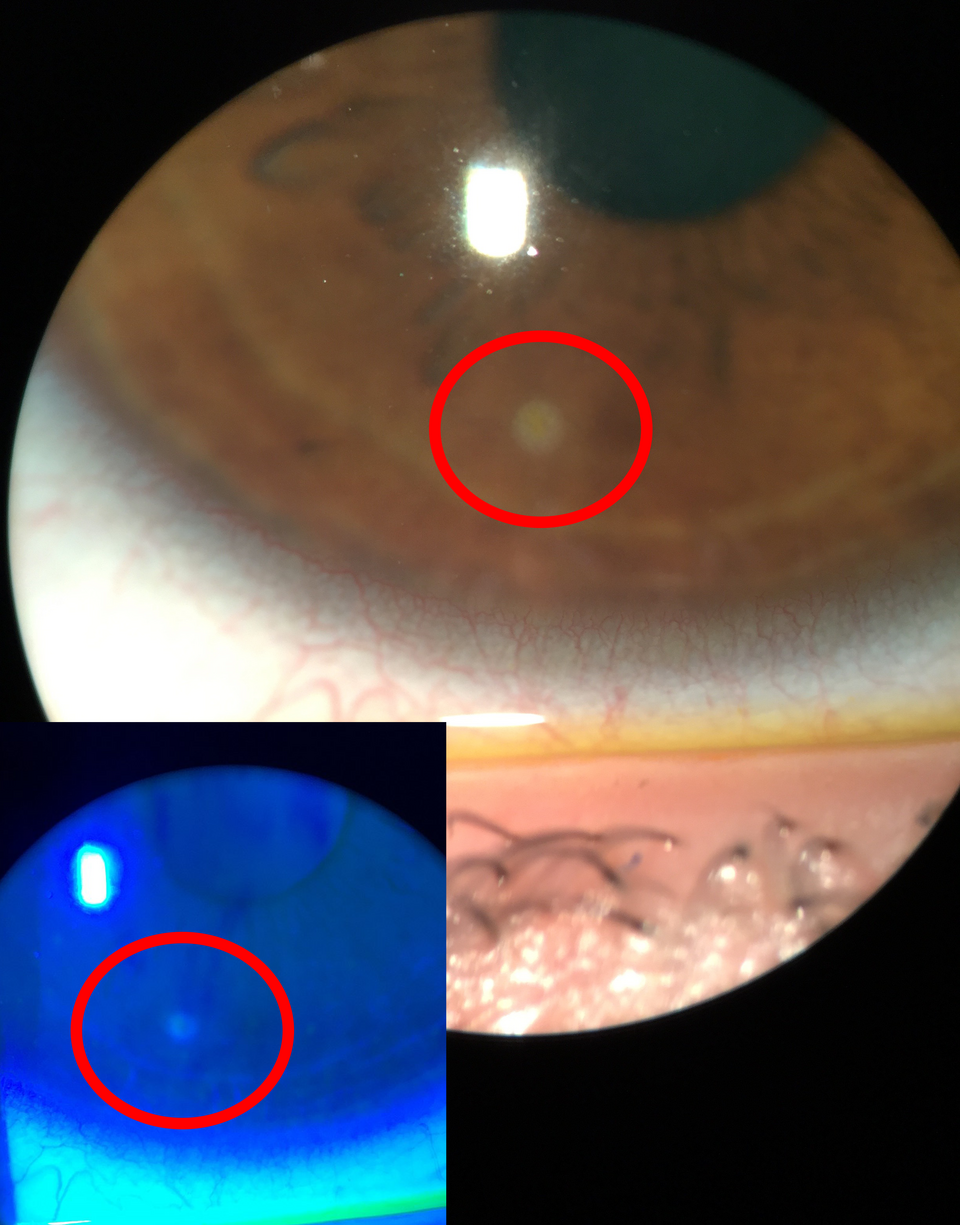
An eye doctor (optometrist or ophthalmologist) examines your eye with a slit-lamp microscope. Common steps include:
- Fluorescein dye to highlight any corneal defect or ulcer
- Vision check and anterior chamber exam for cells/flare or hypopyon
- Corneal scrapings/cultures for severe, large, central, or unusual ulcers (identify bacteria, fungi, or Acanthamoeba)
- Review of lens habits and sometimes culturing the lens, case, or solution
Fast diagnosis and close follow-up protect vision and reduce scarring. 6 7
Treatment and Management
Goals: clear infection, reduce inflammation, and protect the cornea from scarring or perforation. Plans depend on the germ, ulcer size/location, and vision.
- Immediate steps: Stop wearing lenses; do not patch the eye; avoid lenses until cleared.
- Antibiotic eye drops: Most bacterial ulcers use frequent topical antibiotics (often a fluoroquinolone); very severe ulcers may need fortified drops. Evidence supports topical antibiotics as first-line therapy. 8
- Other infections: Suspected Acanthamoeba may need biguanides (e.g., PHMB or chlorhexidine) for weeks; fungi need antifungals (e.g., natamycin or voriconazole). Therapy is tailored to tests and exam.
- Pain & inflammation: Cycloplegic drops help light sensitivity. Steroid drops may be considered only after bacterial control and with specialist guidance; early use in selected bacterial cases can help but is individualized. 9
- Follow-up: Frequent visits (often daily initially) to monitor healing and adjust treatment; severe cases may need hospitalization, glue, or surgery if perforation risk develops.
- When to culture: Large, central, deep, atypical, or poorly responding ulcers are commonly cultured to guide therapy.
Living with Contact Lens Keratitis and Prevention
Healing takes days to weeks. Scars may leave a faint spot; central scars can blur vision. Treat early—and prevent the next episode:
- Never sleep in lenses unless prescribed as extended wear.
- Keep water away: no showering, swimming, or hot tubs in lenses; never rinse lenses/cases with tap water. 10
- Rub and rinse every time (unless daily disposables). Use fresh solution; no topping off. Replace case at least every 3 months. 11
- Follow replacement schedules; consider daily disposables if care steps are hard.
- Take breaks with glasses if eyes feel irritated.
- Call sooner for pain, redness, or blur—remove the lens and contact the clinic.
Good habits plus regular exams make contact lens wear safer and more comfortable.
Latest Research & Developments
Trends in organisms & care systems: Reviews of contact lens–associated bacterial keratitis highlight common bacteria such as Pseudomonas aeruginosa and Staphylococcus, and the roles of lens type and hygiene. Research explores lens materials, daily disposable wear, and hydrogen peroxide systems to reduce risk. 12
Smarter testing: Culturing corneas, lenses, and cases helps match treatment to organisms and local resistance; faster diagnostics (e.g., PCR) are being studied to identify germs earlier. 13
Recent Peer-Reviewed Research
Immune defense single nucleotide polymorphisms and recruitment strategies associated with contact lens keratitis.
Carnt NA, Willcox MD, Hau S, et al.
Association of single nucleotide polymorphisms of interleukins-1β, -6, and -12B with contact lens keratitis susceptibility and severity.
Carnt NA, Willcox MD, Hau S, et al.
Risk factors for the development of corneal infiltrative events associated with contact lens wear.
Morgan PB, Efron N, Brennan NA, et al.
Next Steps
Urgent: If you suspect contact lens keratitis, remove lenses and seek same-day care. A cornea specialist is ideal, though many optometrists and general ophthalmologists can start treatment and coordinate referral.
- How to schedule: Ask for a “same-day urgent eye visit for a painful red eye in a contact lens wearer.” Bring glasses, the lens case, actual lenses, and solutions (they may be cultured).
- What to expect: You’ll likely start antibiotic drops immediately and need frequent follow-up early on.
- If appointments are full: Request the cancellation list, try urgent care attached to an eye clinic, or ask your primary care office to help expedite. Severe pain/vision loss may warrant the emergency department.
For safety tips on healthy lens wear and care, see the CDC pages. 14
Trusted Specialists
Board-certified providers specializing in Contact Lens Keratitis.
