Bacterial Keratitis
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
Bacterial keratitis is an infection of the cornea—the clear, curved "window" at the front of the eye. Germs (most often Pseudomonas aeruginosa or Staphylococcus aureus) can rapidly cause pain, redness, light sensitivity, and blurred vision. Without fast treatment, scarring or even loss of the eye can occur. Risk rises with contact lens wear, eye injury, or a weak eye surface. Early care usually leads to better results. 1
Doctors may call a severe bacterial corneal infection a "corneal ulcer". These terms are related but not always identical. What matters most is getting help quickly if you notice symptoms. 2
Symptoms
Symptoms can start suddenly and worsen over hours to days. Common signs include:
- Eye pain (sharp or aching)
- Redness and tearing
- Light sensitivity (photophobia)
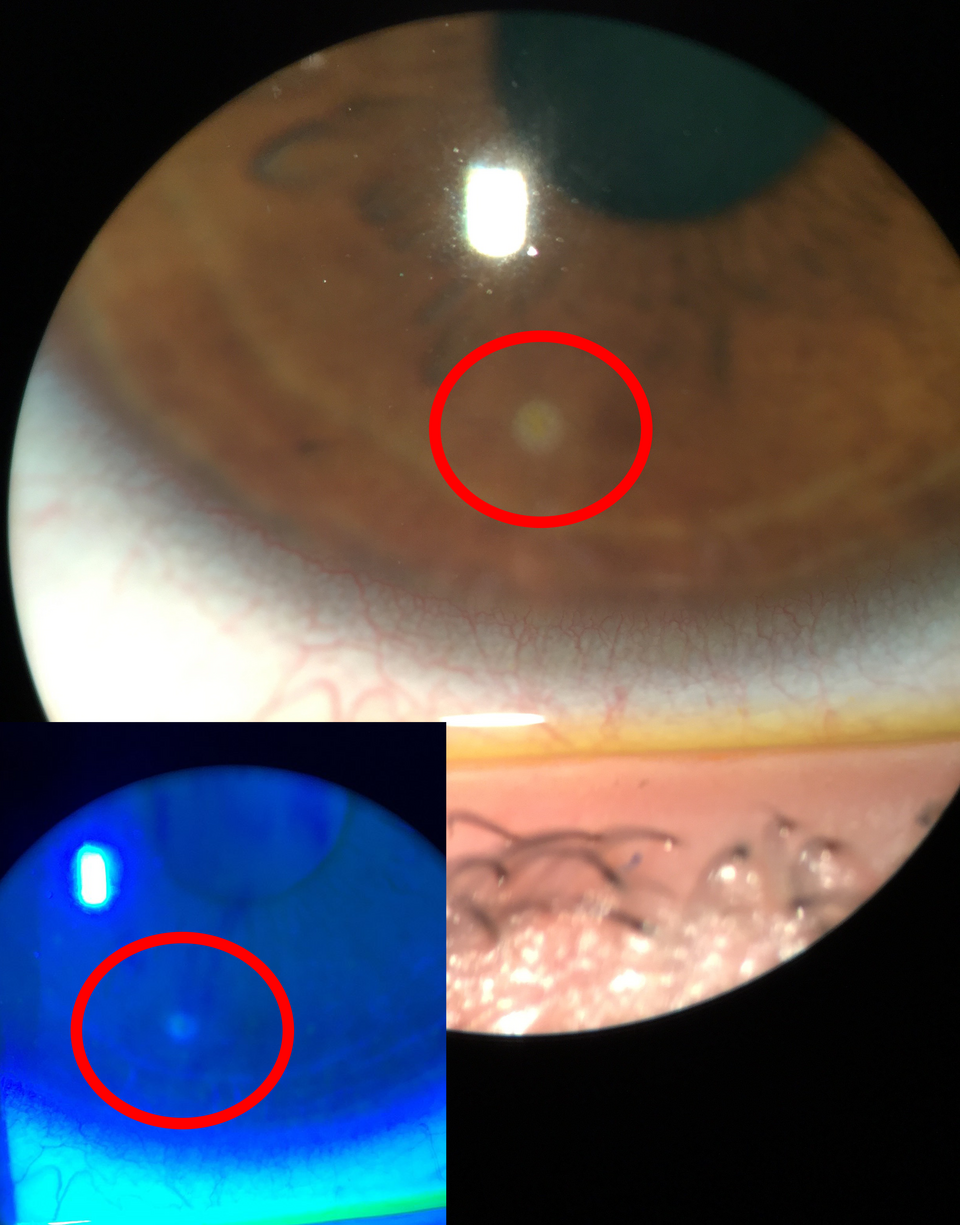
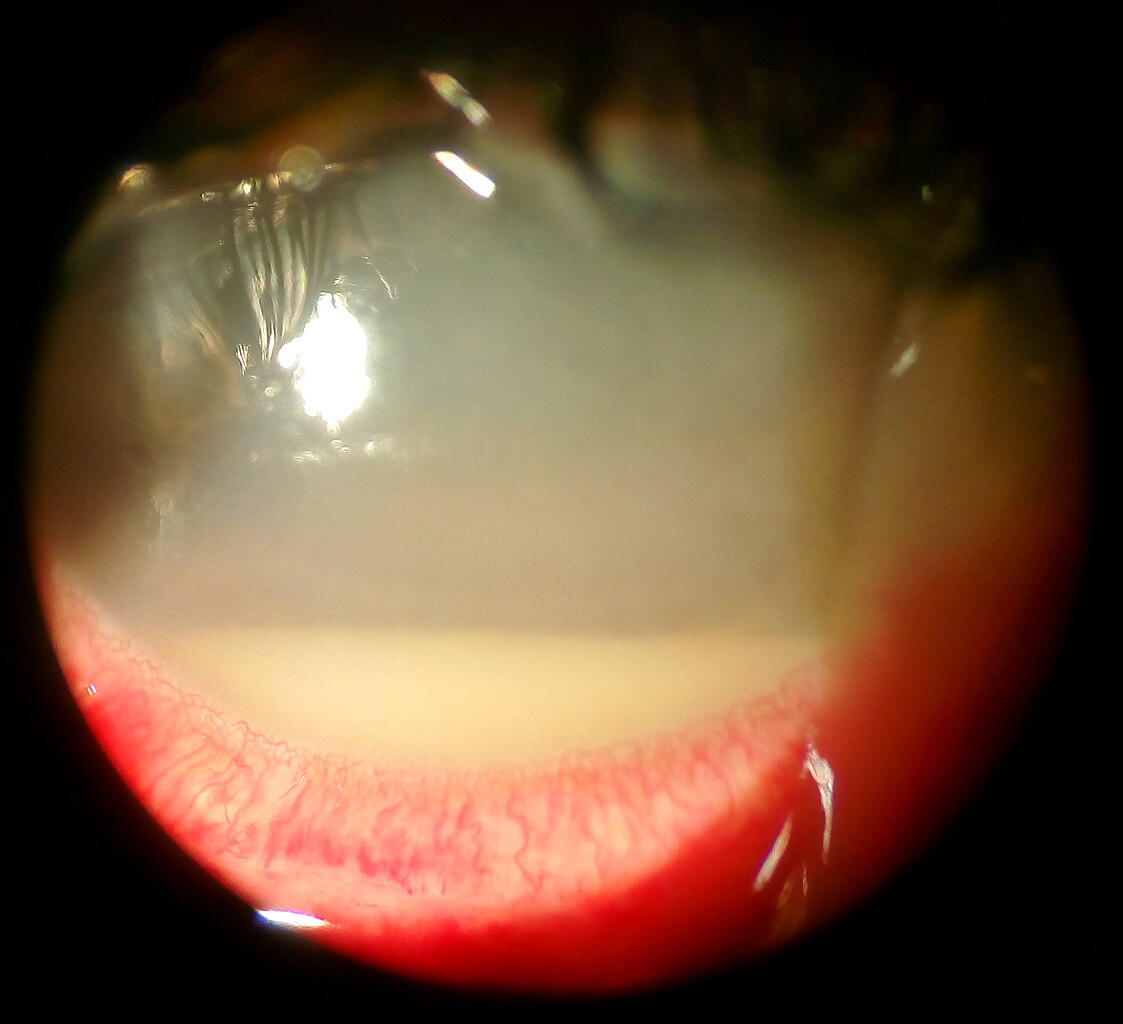
- Blurry vision or a gray/white spot on the cornea
- Discharge or crusting of the lashes
In more serious cases, white cells can settle in the front of the eye (hypopyon). If you wear contact lenses, remove them and seek care the same day if these signs appear. 2 3
Causes and Risk Factors
Bacteria enter through tiny breaks in the corneal surface—often with contact lens wear, small scratches, or dry/unhealthy ocular surfaces. Common germs include Pseudomonas and Staphylococcus.
Risks you should know:
- Contact lenses (especially sleeping, swimming, or showering in lenses; poor cleaning)
- Trauma (scratch from a branch or foreign body)
- Surface problems (dry eye, eyelid issues, previous surgery)
- Topical steroids without close supervision
- Health conditions that reduce healing
Contact lens wear is a major risk in many countries, and Pseudomonas infections are strongly linked to lens wear. 1 4
Bacterial Keratitis: Simple Severity & Urgency Score (Assumption-Based)
Select your details to estimate risk factors.
Diagnosis
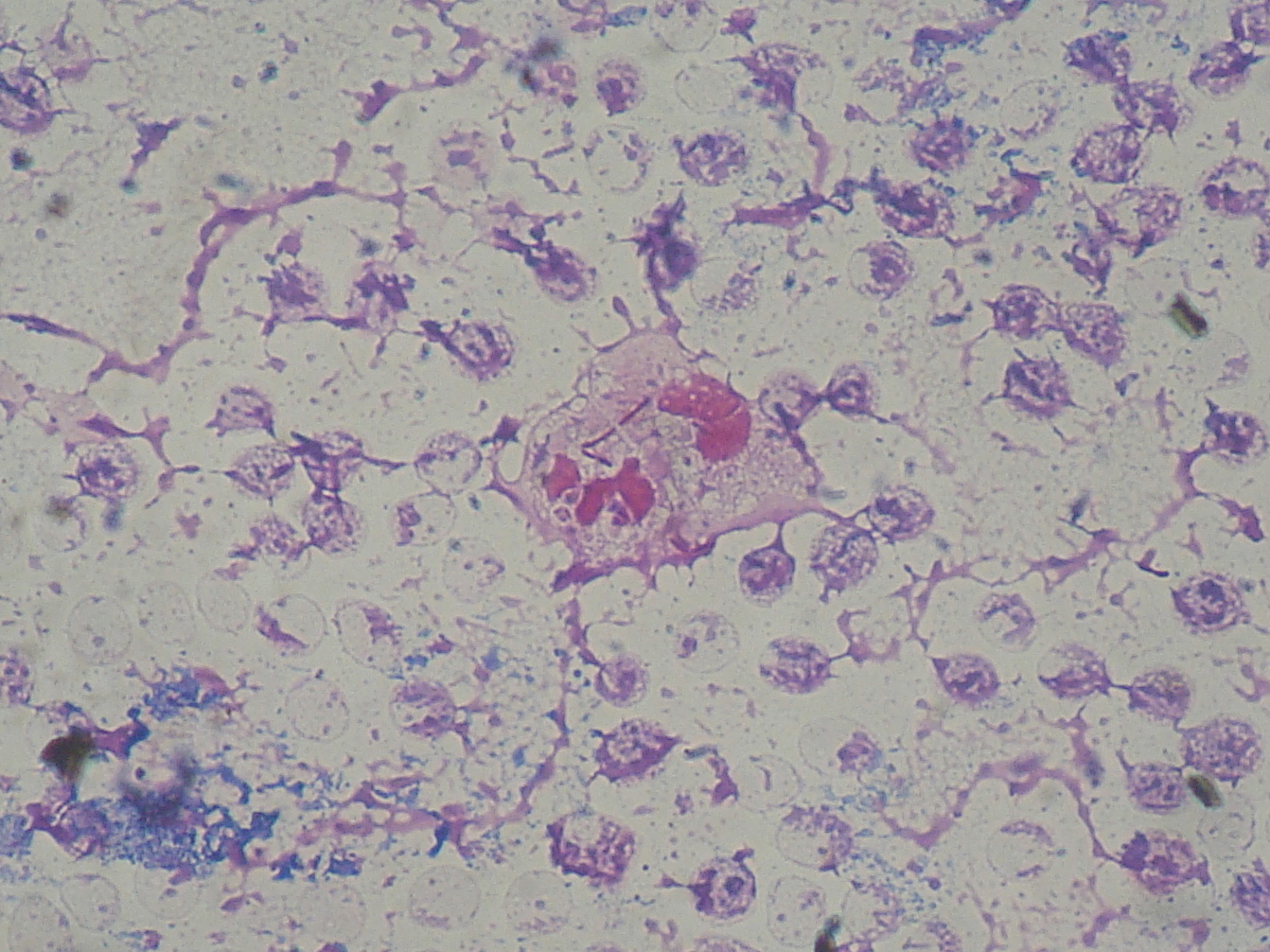
An eye doctor (ophthalmologist or optometrist) will examine your eye with a slit-lamp microscope. Typical steps include:
- History: contact lens habits, any injury, timing of symptoms
- Slit-lamp exam: corneal infiltrate/ulcer, surface defect with dye, presence of hypopyon
- Vision check and photographs to track healing
- Scraping for stain/culture in moderate–severe cases, unusual patterns, or if worsening—cultures target the best antibiotic
Doctors may also check eye pressure and look for thinning or perforation risks. Prompt diagnosis guides the right drops and dosing. 2 3
Treatment and Management
Antibiotic eye drops are the mainstay. Choice depends on ulcer size, location, appearance, and risk factors.
- First-line therapy: Many small, peripheral ulcers are treated with strong fluoroquinolone drops (e.g., moxifloxacin) used very frequently at first, then tapered.
- Fortified antibiotics: Large, deep, central, or sight-threatening ulcers often need specially mixed (fortified) drops such as tobramycin plus a cephalosporin or another agent, sometimes alternating every 30–60 minutes initially.
- Cycloplegic drops may reduce pain and light sensitivity.
- Avoid contact lenses until fully healed and cleared by your doctor.
Steroid drops? Not started at the beginning. In select cases, a physician may add a steroid after antibiotics have begun and the infection shows control (e.g., SCUT trial), but this is individualized and not for everyone. 4 5
When to culture or refer urgently: Very large or central ulcers, worsening cases, or infections after plant-matter trauma often need cultures, more frequent visits, and sometimes hospital-level care. Your doctor will give exact drop schedules and follow-up timing.
Living with Bacterial Keratitis and Prevention
Most people recover with quick, steady care—but scarring can occur. Protect your eyes and lower recurrence risk:
- Follow your drop plan exactly; bring bottles to visits
- Rest eyes; avoid dusty/dirty environments while healing
- Do not wear contact lenses until cleared
- Use eye protection during sports and yardwork
Contact lens hygiene tips:
- Wash/dry hands before handling lenses
- Rub and rinse as directed; use fresh solution—never water or saliva
- No sleeping, swimming, or showering in lenses unless specifically allowed
- Replace cases regularly and follow wear schedules
Good lens care and regular eye exams reduce bacterial keratitis risk and protect vision. 1 3
Latest Research & Developments
Which antibiotics work best? Evidence compares fluoroquinolone monotherapy with fortified combinations for moderate–severe ulcers. Both are used; the optimal choice depends on local resistance and ulcer severity—care is individualized. 6
Contact lens trends & resistance: Ongoing surveillance of organisms/resistance in lens-associated infections informs smarter first-line therapy. 7
New directions: Teams are testing ways to reduce harmful inflammation and speed healing in difficult ulcers, including work supported by the U.S. National Eye Institute. 8
Recent Peer-Reviewed Research
Steroids and Cross-Linking for Ulcer Treatment: The SCUT II Randomized Clinical Trial.
Prajna NV, Lalitha P, Chandru S, et al.
Hyperglycemia-Suppressed Acod1 Expression Contributes to Innate Immune Deficiency in Pseudomonas aeruginosa Keratitis.
Gao N, Me R, Singh S, et al.
Tectonic Corneal Transplant in the Management of Congenital Anterior Staphyloma.
Rodrigues R, Scanga H, Potluri P, et al.
Next Steps
If you think you have a corneal infection, seek care today. A cornea specialist (ophthalmologist) is ideal, but many urgent clinics and optometrists can start evaluation and coordinate with a cornea expert.
- How to schedule: Say, “I have painful red eye and blurry vision—possible corneal ulcer.” Ask for the soonest appointment and the cancellation list.
- What to bring: Contact lens case/solution, all eyedrops, and any recent records/photos.
- Referrals & follow-up: Some plans need a referral—check with your primary clinic. Expect frequent early follow-ups.
Regular checkups and eye-safe habits lower future risk. 3
Trusted Specialists
Board-certified providers specializing in Bacterial Keratitis.
