Central Serous Retinopathy
Also known as CSR
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.


Overview
Central serous retinopathy (CSR), also called central serous chorioretinopathy, is a condition in which fluid from the layer of blood vessels under the retina (the choroid) leaks through a microscopic defect in the retinal pigment epithelium (RPE). That leakage forms a blister-like pocket of fluid beneath the macula, the part of the retina that gives sharp central vision. People often notice a dark smudge, distorted or shrunken objects, or dulled colors in one eye. Most acute episodes clear spontaneously within 1–3 months, but chronic or recurrent disease can leave permanent scarring and vision loss.1 CSR is the fourth-most-common macular disorder after age-related macular degeneration, diabetic retinopathy, and vein occlusion, and it disproportionately affects healthy men between 30 and 50 who report high stress levels or recent corticosteroid use.2
Symptoms
CSR may arise suddenly or insidiously and usually involves only one eye at first. Classic complaints include:
- Blurry or dim central vision that looks like a gray or brown spot.
- Metamorphopsia – straight lines appear wavy or bent.1
- Micropsia – objects seem smaller or farther away.
- Dull or washed-out colors, especially first thing in the morning.
- Reduced contrast sensitivity and trouble reading fine print.4
Because peripheral vision stays clear and pain is absent, some people overlook early symptoms until a routine eye exam uncovers the detachment.
Causes and Risk Factors
The exact trigger remains under investigation, but several well-documented risk factors make the underlying choroidal vessels more likely to leak:
- Endogenous or exogenous corticosteroids – pills, inhalers, nasal sprays, skin creams, or systemic stress hormones raise the odds up to 37-fold.2
- Psychological stress and “type A” personality that elevate circulating cortisol.1
- Male sex (≈ 70–80 % of cases) and age 30–50.
- Obstructive sleep apnea, hypertension and heart disease – conditions that impair choroidal perfusion.4
- Helicobacter pylori infection, pregnancy, phosphodiesterase-5 inhibitors, and anabolic-steroid or testosterone supplements.
Central Serous Retinopathy Risk Score
Select your details to estimate risk factors.
Diagnosis
A retina specialist confirms CSR with in-office imaging:
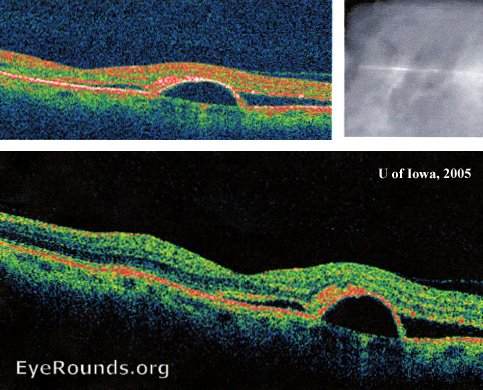
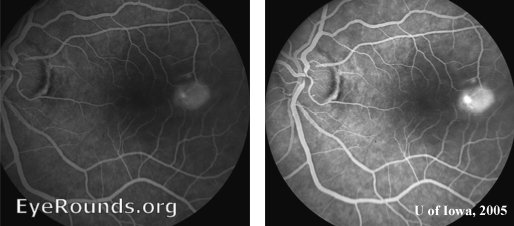
- Optical coherence tomography (OCT) shows a dome-shaped elevation of neurosensory retina and often a thicker-than-normal choroid.3
- Fluorescein angiography (FA) reveals a characteristic “ink-blot” or “smoke-stack” leakage pattern.
- Indocyanine-green angiography can highlight dilated pachy-choroidal vessels in chronic cases.
- Visual-acuity and Amsler-grid testing document baseline function.
- Targeted review of medications and blood pressure helps uncover modifiable triggers.1
Routine lab work is unnecessary unless systemic inflammatory or infectious disease is suspected.
Treatment and Management
Watchful waiting is appropriate for a first attack because >80 % of patients recover close-to-baseline vision without intervention. Your retina doctor will typically re-image the eye at 4–6-week intervals. Evidence-based options for persistent (>3 months) or chronic CSR include:
- Discontinuing or tapering corticosteroids whenever safely possible.1
- Half-dose or half-fluence photodynamic therapy (PDT) with verteporfin to seal the leak while sparing surrounding retina – now considered first-line for chronic disease.4
- Sub-threshold micropulse laser aimed at extra-foveal leak sites.
- Mineralocorticoid-receptor antagonists (eplerenone or spironolactone) in selected patients under internist supervision.
- Anti-VEGF injections if secondary choroidal neovascularization develops.
Acute vision that drops below driving standards, bilateral involvement, or failure to improve after three months usually prompts active treatment.
Living with Central Serous Retinopathy and Prevention
Most people eventually regain useful vision, but recurrence occurs in up to half of patients. Practical self-care tips include:
- Identify and lower stressors through exercise, mindfulness, counseling, or schedule adjustments.2
- Avoid unnecessary steroids; discuss alternatives with your prescribing physicians.1
- Treat sleep apnea and aim for 7–8 hours of quality sleep nightly.
- Monitor vision at home with an Amsler grid; report new distortion promptly.
- Use protective eyewear during sports to prevent traumatic macular damage.
Most patients resume normal work within days but may need temporary lighting adjustments or magnifiers for fine print until fluid clears.
Latest Research & Developments
Research into CSR focuses on choroidal blood-flow regulation and therapies that avoid collateral retinal damage:
- Pachychoroid imaging studies using enhanced-depth OCT reveal that a thick, hyper-permeable choroid precedes many chronic cases and may guide earlier, lower-dose PDT.3
- Randomized trials of eplerenone vs. sham are under way after pilot studies showed faster fluid resolution and fewer recurrences.4
- Low-energy, 577-nm micropulse laser protocols aim to treat leaks within the foveal avascular zone without creating visible burns.
- AI-based OCT analytics are being trained to predict which acute cases will become chronic, potentially personalizing follow-up intervals.
- Gene-association projects are exploring whether polymorphisms in mineralocorticoid-receptor pathways predispose patients to steroid-triggered CSR.
Recent Peer-Reviewed Research
Choroidal Melanoma Masquerading as Central Serous Chorioretinopathy.
Negretti GS, Kalafatis NE, Shields JA, et al.
Nondamaging photothermal therapy for the retina: initial clinical experience with chronic central serous retinopathy.
Lavinsky D, Palanker D
Bilateral subfoveal neurosensory retinal detachment associated with MEK inhibitor use for metastatic cancer.
McCannel TA, Chmielowski B, Finn RS, et al.
Next Steps
If your vision distortion lasts more than a week, worsens, or affects both eyes, schedule promptly with a retina specialist. These ophthalmologists have advanced training in macular imaging, laser safety, and photodynamic therapy.
How to schedule: A primary eye-care provider can refer you, but many retina clinics accept self-referrals; urgent appointments are typical for sudden vision loss. You can also connect directly to a fellowship-trained retina expert through Kerbside to review imaging, discuss medication risks, or arrange PDT without long waits.14