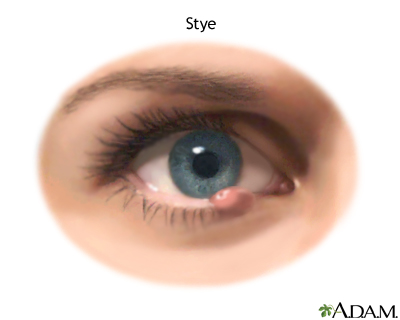
Stye and Chalazion
Also known as Hordeolum, Eyelid Bump
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.


Overview
Styes (external or internal hordeola) are acutely infected oil glands along the lash line, while a chalazion is a slow-growing, sterile lump that forms when a gland’s inflamed contents become walled off. Both appear as eyelid bumps, but styes usually hurt and come on fast, whereas chalazia are typically painless and linger for weeks.1 Each year millions of people develop at least one eyelid bump; most resolve with warm compresses, but some require office-based procedures. Prompt recognition prevents vision-threatening complications and unnecessary antibiotic use.2
Symptoms
Common warning signs include:
- Red, tender nodule at the lash line (stye) or deeper in the lid (chalazion).
- Localized swelling, tearing, gritty sensation, and light sensitivity.1
- Yellow point or spontaneous drainage as a stye “comes to a head.”
- Blurred vision or heavy-lid feeling if a large chalazion presses on the cornea.3
Seek urgent care if swelling spreads beyond the eyelid or you develop fever—signs of pre-septal or orbital cellulitis.
Causes and Risk Factors
Styes start when Staphylococcus aureus infects a blocked lash (gland of Zeis) or meibomian gland. Chalazia arise from unresolved inflammation. Factors that raise risk include:
- Chronic blepharitis or meibomian-gland dysfunction that leaves oily debris along the lids.5
- Poor eyelid hygiene, heavy eye-make-up, or infrequent replacement of cosmetics.
- Rosacea, seborrheic dermatitis, diabetes, high cholesterol, and smoking.
- Contact-lens overwear or handling lenses with unwashed hands.4
Stye/Chalazion Risk Score
Select your details to estimate risk factors.
Diagnosis
An experienced clinician can usually make the diagnosis at the slit lamp:
- Stye: focal pustule on the lid margin that is tender to touch.
- Chalazion: firm, movable nodule within the tarsal plate; everted lid reveals a grayish granuloma.
- Rule-outs: sebaceous-cell carcinoma, basal-cell carcinoma, and pre-septal/orbital cellulitis.2
- If atypical, biopsy or imaging may be ordered to exclude malignancy.6
Treatment and Management
First-line home care
- Apply a clean, moist warm compress 10–15 minutes, 3–5 times daily to liquefy trapped oil.3
- Perform gentle lid scrubs with diluted baby shampoo or commercial eyelid wipes.
- Discontinue eye make-up and replace old mascara or eyeliner.
Medical therapy
- Topical antibiotic ointment (e.g., bacitracin/polymyxin) if crusting or discharge is present.4
- Oral doxycycline for recurrent chalazia linked to rosacea.
Office procedures
- Incision & curettage (I&C) for lesions persisting >4–6 weeks.
- Intralesional steroid (triamcinolone) injection when I&C is contraindicated.
Most styes drain within a week; chalazia may take a month or longer to resolve.
Living with Styes / Chalazia and Prevention
You can lower the chance of flare-ups by:
- Daily lid-margin hygiene: after warm compress, massage the lid toward the lashes, then clean with a cotton swab and diluted baby shampoo.
- Replace eye cosmetics every 3 months and avoid sharing them.
- Follow contact-lens hygiene rules—wash hands, rub-and-rinse lenses, and never sleep in daily-wear lenses.6
- Control blepharitis and skin conditions such as rosacea and seborrhea.5
Call your eye-care provider if lumps enlarge, recur frequently, or impair vision.
Latest Research & Developments
Exciting advances are emerging for stubborn eyelid-gland disease:
- Stem-cell signaling: 2025 NEI-funded work identified Hedgehog pathway decline as a driver of age-related meibomian-gland atrophy—opening the door to regenerative therapies.7
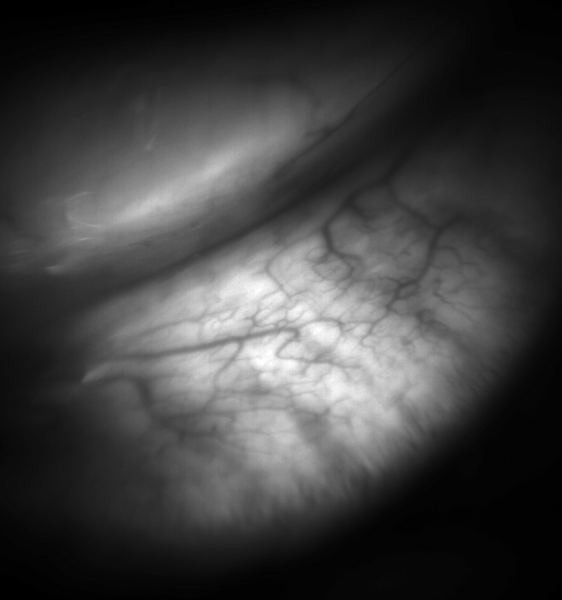
- Artificial-intelligence meibography: A 2022 deep-learning model accurately segmented glands and removed glare, paving the way for objective monitoring of stye/chalazion risk.8
- Heat-pulsation masks & intense-pulsed-light devices continue to improve gland patency and shorten recovery times in early trials.
Recent Peer-Reviewed Research
Meibum and lid margin microbiome in eyes with chalazion: exploring an infectious aetiology.
Singh S, Maity M, Arunasri K, et al.
Effectiveness of smartphone technology for detection of paediatric ocular diseases-a systematic review.
Vijendran S, Alok Y, Kuzhuppilly NIR, et al.
Pediatric blepharokeratoconjunctivitis: findings and outcomes in Hispanic vs. Non-Hispanic patients.
Wilberding M, Bolton EM, Bohnsack B, et al.
Next Steps
If a bump has not improved after two weeks of diligent warm compresses—or if it repeatedly comes back—ask your optometrist or family doctor to refer you to an oculoplastic surgeon (an ophthalmologist who specializes in eyelids). Same-week appointments are usually available for potential infections or surgical drainage.
You can also connect directly with the right specialist through Kerbside for tailored advice and, when needed, rapid scheduling of in-office procedures. Bring a list of tried treatments, current medications, and photos of the bump’s evolution to streamline the consultation.12