Fungal Keratitis
Also known as Keratomycosis
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms for details.
Overview
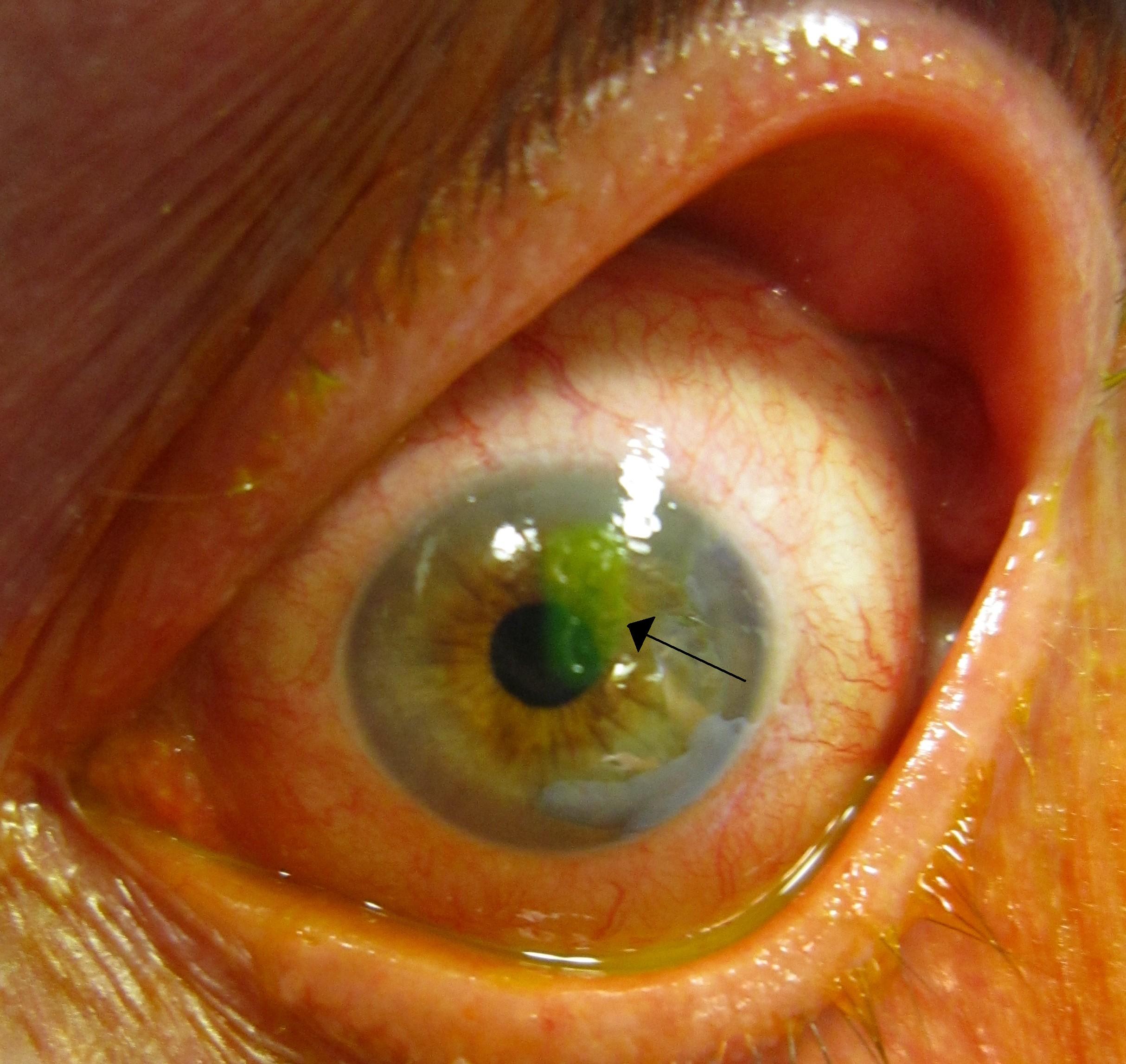
Fungal keratitis is an infection of the cornea, the clear front window of the eye. It happens when fungi (like Fusarium, Aspergillus, or Candida) enter the cornea and begin to grow. This can follow an eye injury, contact lens problems, or eye surgery. It is serious and can threaten sight if not treated quickly 1.
Fungal eye infections can cause pain, light sensitivity, redness, tearing, and blurry vision. They may develop over days to weeks after the eye is injured, especially by plant material such as a thorn or stick. Early diagnosis and treatment improve the chance of healing and protecting vision 2.
Symptoms
Symptoms often resemble other corneal infections. Call your eye doctor right away if you notice:
- Eye pain, redness, or a feeling something is in the eye
- Light sensitivity (bright light hurts)
- Blurred vision or a white/gray spot on the cornea
- Tearing or discharge
Contact lens wearers may feel more irritation when the lens is in place. Anyone with these symptoms after an eye injury should be checked urgently 2 3.
Causes and Risk Factors
Fungal keratitis starts when fungi enter the cornea through a tiny scratch or surface break. This can happen after:
- Eye injury with plant material (thorns, branches, grain)—a classic trigger, especially in farm or outdoor work
- Contact lens issues: poor hygiene, sleeping in lenses not approved for overnight use, or rinsing with tap water
- Recent eye surgery or chronic corneal surface problems
- Health factors: diabetes, weakened immune system, or steroid use (can raise risk and slow healing)
Good news: many risks are preventable with eye protection and healthy lens habits 2 4.
Fungal Keratitis: Simple Risk of Poor Outcome (Assumption-Based)
Select your details to estimate risk factors.
Diagnosis
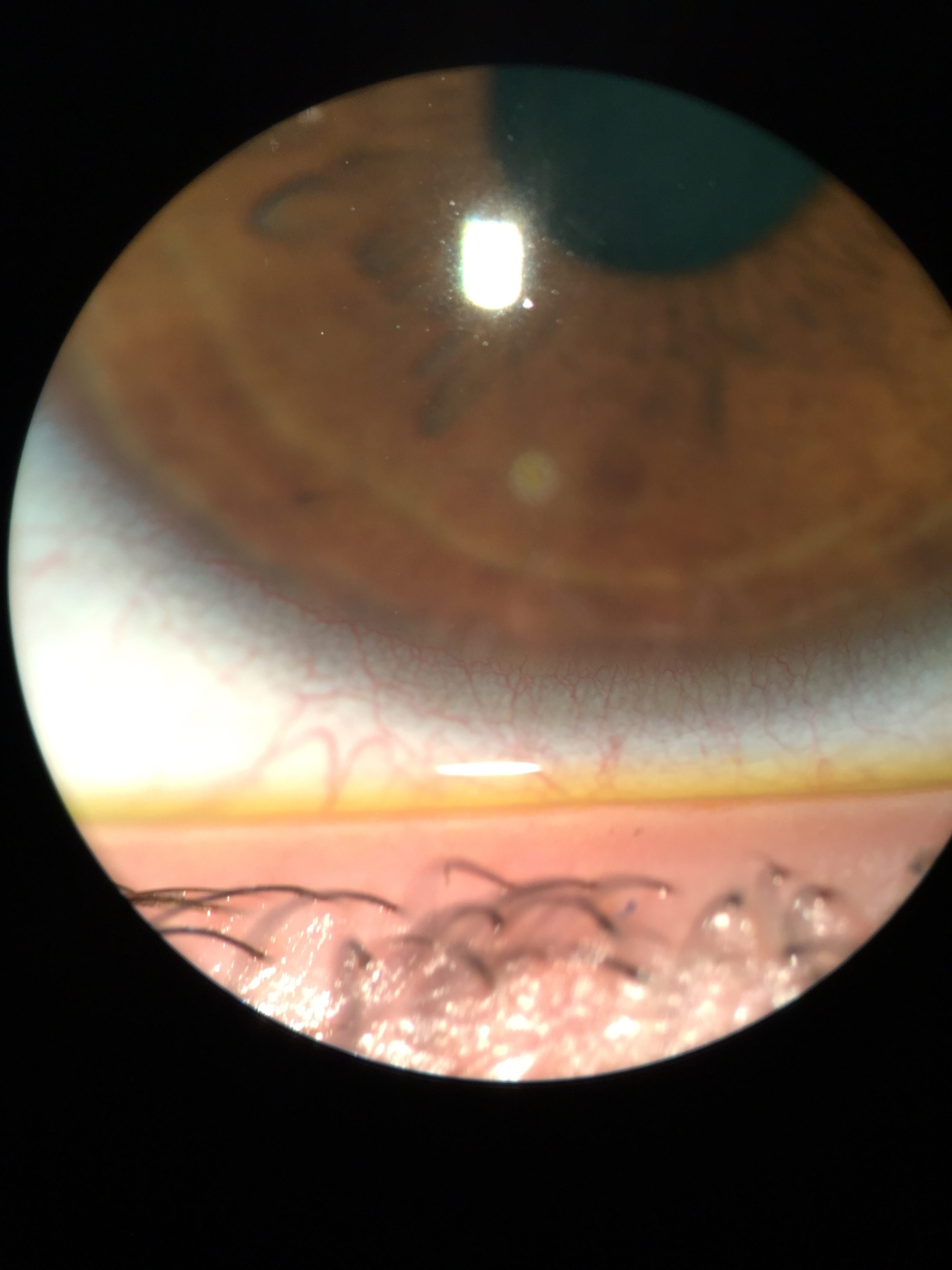
An eye doctor (ophthalmologist) examines the eye with special lights and may use fluorescein dye to highlight the ulcer. To confirm fungus, the doctor often takes a small corneal scraping and sends it for testing:
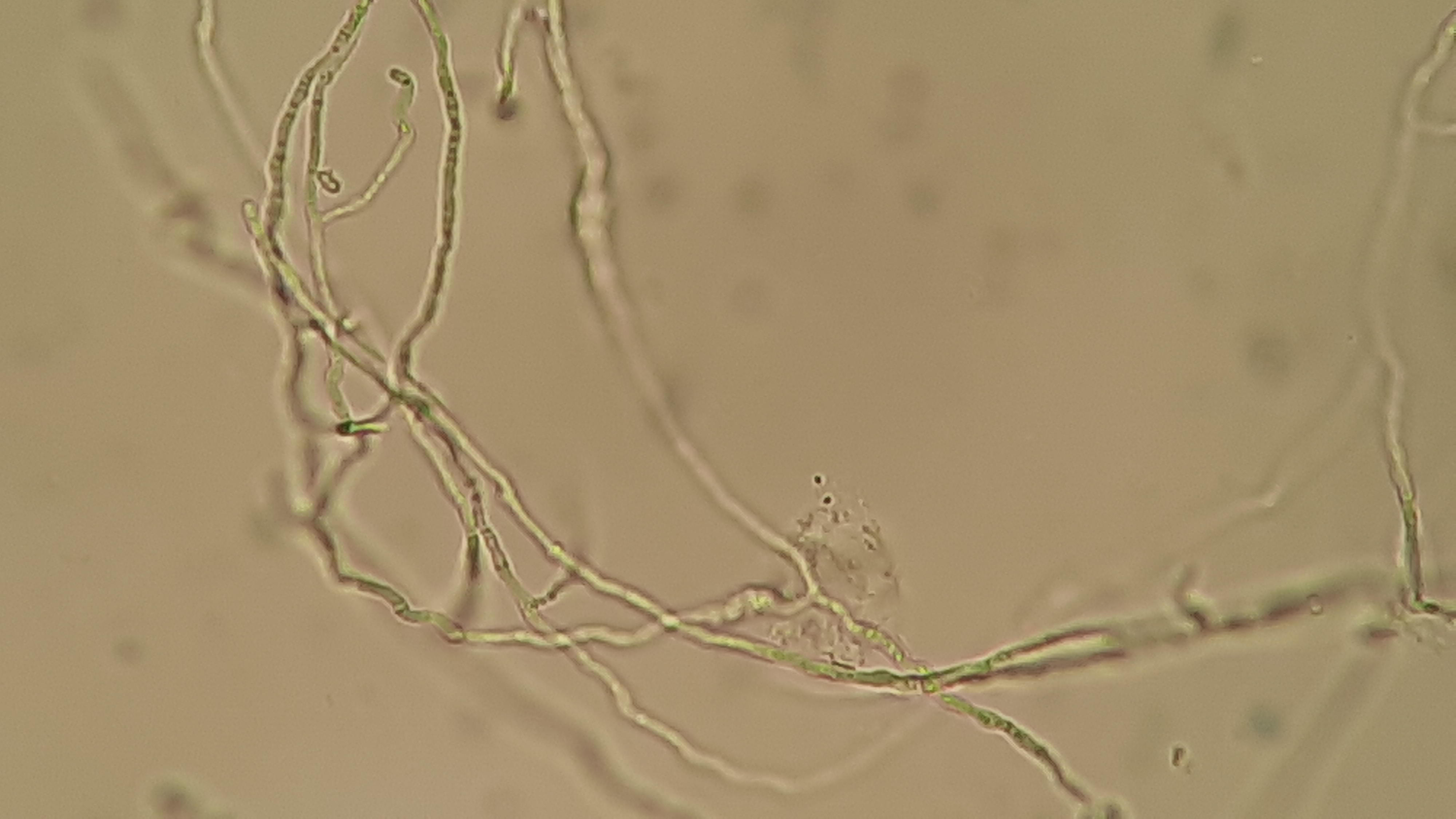
- Microscopy/stains (e.g., KOH prep) to show fungal filaments
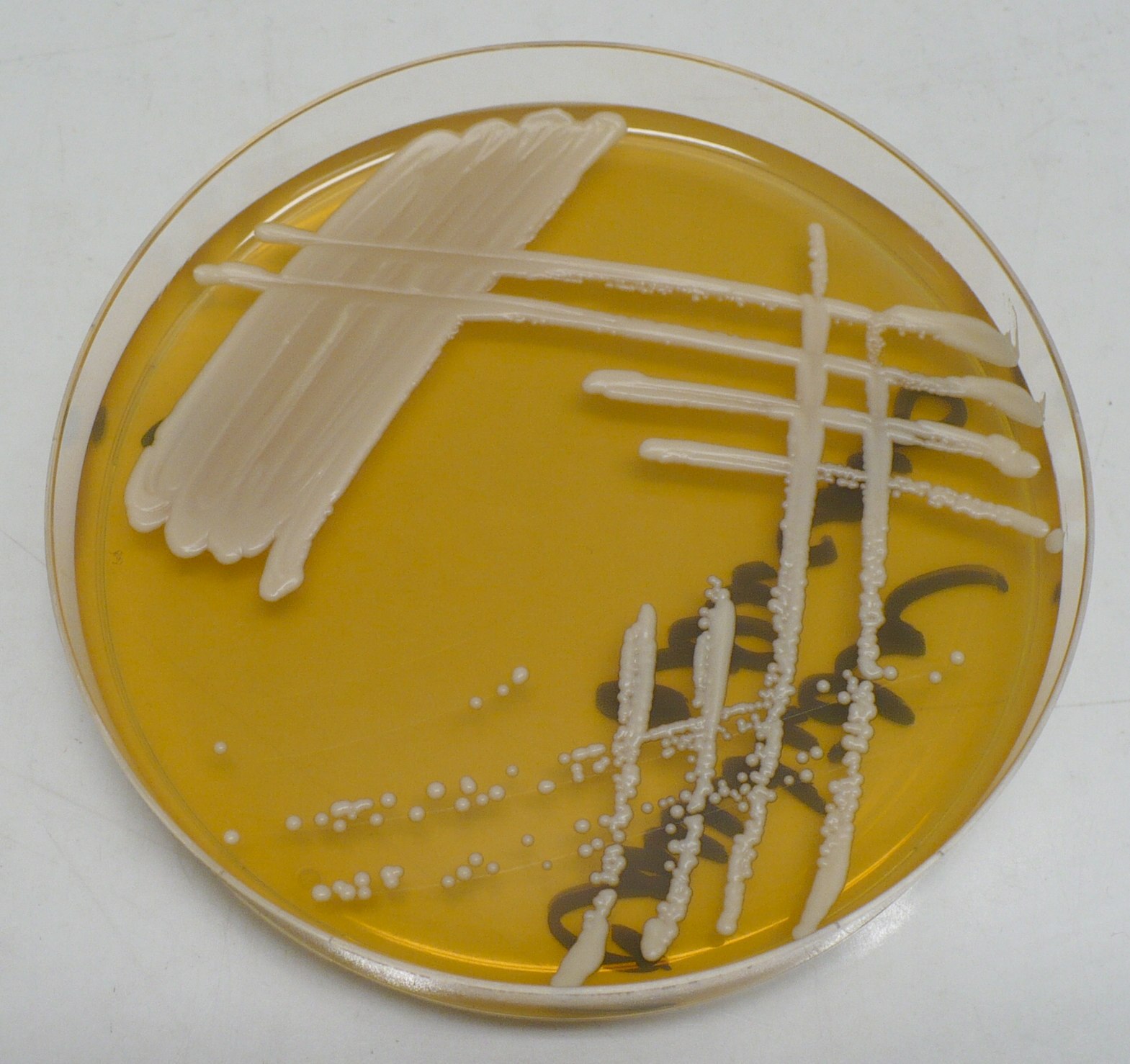
- Culture on special media (e.g., Sabouraud dextrose agar) to identify the organism and guide treatment
- In some centers, confocal microscopy or PCR for faster results
Because fungal growth can be slow, the doctor may start treatment based on the exam while tests are processing. Close follow-up is important to watch healing and intraocular pressure 5 2.
Treatment and Management
Goals: kill the fungus, reduce inflammation, and prevent scarring or perforation. Your doctor will tailor therapy based on organism, size, depth, and location of the ulcer.
- Antifungal eye drops: Natamycin 5% (only FDA-approved topical antifungal for eyes) is often first choice, especially for filamentous fungi like Fusarium. Amphotericin B 0.15% is commonly used for yeasts (e.g., Candida). Voriconazole 1% may be added in select cases. A large trial found natamycin led to better vision and fewer perforations than voriconazole for filamentous infections, especially Fusarium 6 5.
- Oral or injected antifungals for deep, severe, or spreading disease
- Supportive care: pain control, protective shield, and sometimes a dilating drop to rest the iris
- Avoid early steroid drops unless your cornea specialist advises—steroids can worsen fungal infection
- Surgery: if the ulcer threatens to perforate or fails medical therapy, a therapeutic keratoplasty (corneal transplant) may be needed
Costs & price (practical tips)
- Drops: Ask about generics and 90-day supplies. Some antifungals are compounded—request a price quote and check coverage.
- Frequent dosing: Early treatment may require hourly dosing; ask for a written schedule and help at home.
- Insurance: For outpatient procedures and imaging, request a pre-estimate. For potential surgery, ask for a bundled estimate (surgeon, facility, anesthesia) and verify in-network status.
- Assistance: Consider manufacturer programs, pharmacy discount cards, and mail-order options.
Your specialist will adjust the plan based on test results and response 5.
Living with Fungal Keratitis and Prevention
Most people heal with the right care, but recovery can take weeks. To protect vision:
- Take every dose of drops exactly as prescribed (use phone alarms and a written schedule)
- Keep follow-ups—early care often requires frequent visits
- Protect the eye from bumps, dust, and bright light; use a shield as directed
- Contact lens care: do not wear lenses until cleared; later, follow strict hygiene and never rinse with tap water
- Prevent injuries: wear safety glasses for yardwork, farm work, or tasks with flying plant material
Healthy habits, fast care after injuries, and smart lens hygiene lower infection risk and help healing 2 4.
Latest Research & Developments
Natamycin vs. voriconazole: The Mycotic Ulcer Treatment Trial (MUTT) showed natamycin provided better visual outcomes and fewer perforations than voriconazole for filamentous fungal keratitis—especially with Fusarium—supporting natamycin as first-line in many cases 6 7.
Other options & resistance: Ongoing studies examine alternatives (e.g., chlorhexidine vs. natamycin), combinations for difficult infections, and antifungal resistance trends—therapy may be adjusted as evidence evolves 8.
Recent Peer-Reviewed Research
Diagnostic Accuracy of Clinic-Based Loop-Mediated Isothermal Amplification and Quantitative PCR for Fungal and Acanthamoeba Keratitis.
Cao B, Vu CHV, Le CX, et al.
Artesunate Treats Aspergillus fumigatus Keratitis by Inhibiting Fungal Activity and Activating Autophagy Pathway to Reduce Corneal Inflammation.
Liu Y, Tian X, Li C, et al.
Adjunctive Topical Calcineurin Inhibitors During the Treatment of Fungal Keratitis: Practice Patterns and Opinions.
Christy J, Prathikanti V, Abdelrahmen S, et al.
Next Steps
If you think you have fungal keratitis—or were told you might—schedule an urgent visit with a cornea specialist (ophthalmologist).
- How to schedule: Ask for same-day/next-day cornea appointment for suspected corneal ulcer; obtain referral if your plan requires it
- Bring: glasses/contact lens info, medication list, prior records/photos
- Wait-time tips: Request the cancellation list; ask about urgent slots or walk-in cornea clinic; if worsening, go to an emergency eye center
- Prepare: you may be dilated and tested—arrange a ride if light sensitive
For background on corneal conditions, see NEI’s patient pages 9.