Corneal Transplant
also known as Keratoplasty
Last updated August 6, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
A corneal transplant replaces some or all of the eye’s clear front window with healthy donor tissue. Doctors perform the surgery when scarring, swelling, or genetic disease makes the cornea cloudy and light can no longer focus well. More than 80,000 corneal grafts are performed in the United States each year, with success rates exceeding 90 percent for many conditions.1 The National Eye Institute notes that modern lamellar techniques, which swap only diseased layers, have shortened recovery and reduced rejection risk compared with older full-thickness grafts.2
How the Procedure Works & Options
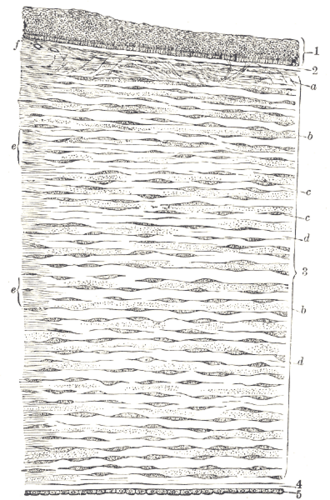
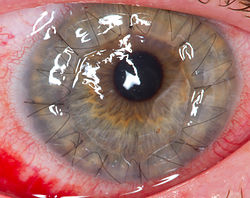
Surgery is done under local or general anesthesia in 30–90 minutes. In penetrating keratoplasty (PK) the surgeon trephines an 8–9 mm “button” of full-thickness tissue and sutures a matching donor button in place. Lamellar options include deep anterior lamellar keratoplasty (DALK) for stromal disease and endothelial techniques (DSAEK, DMEK) for back-layer failure. Endothelial keratoplasty uses a 3 mm incision, air bubbles to position the wafer-thin graft, and often heals without surface stitches.1 Mayo Clinic data show that surgeons choose the least-invasive method that treats the affected layer while preserving healthy tissue.3
Who Is a Candidate?
Adults or children with vision-limiting keratoconus, Fuchs endothelial dystrophy, corneal scars, or swelling that no longer respond to glasses or specialty contacts may benefit. Candidates need a healthy retina and optic nerve so vision can improve after the graft. Active infection, uncontrolled glaucoma, or severe eye surface disease must be treated first. The AAO advises waiting until the eyeglass prescription fluctuates less than 1 diopter over six months, confirming stable corneal shape on topography.1 The NEI adds that most recipients are between 20 and 70 years old, but age alone rarely disqualifies someone.2
Corneal Transplant Readiness Score
Enter your details below to check your suitability for this treatment
Suitability Level
Recommendation
Cost and Price
Charges vary by hospital, surgeon, and region. Analyses of U.S. billing data put the average total cost for a one-eye transplant at USD 16,000 – 32,000, including tissue, surgeon, facility, and anesthesia fees.4 Out-of-pocket expense is usually limited to the deductible and 20 % coinsurance for insured patients, while self-pay packages run USD 10 000 – 18 000 per eye. Mayo Clinic notes that lamellar procedures often qualify for the same coverage and may lower long-term medication costs by reducing steroid needs.3
Benefits and Limitations
Vision commonly improves from counting fingers to 20/40 or better, and graft clarity can last decades. Endothelial keratoplasty patients reach functional vision in weeks rather than months, and DMEK delivers near-normal optics with less induced astigmatism.1 A 10-year multi-center study reported 94 % graft survival for DMEK versus 79 % for conventional PK, with fewer rejection episodes.5 Limitations include months of steroid-drop tapering, possible graft rejection (5–18 %), glaucoma, or infection, and a small risk of graft failure requiring repeat surgery.
Recovery and Long-Term Care
Most patients go home the same day. A clear shield protects the eye, and antibiotic-steroid drops are started four times daily. Endothelial grafts require face-up positioning for several hours so the air bubble can press the tissue flat. Stitches from PK stay in for 12–18 months, while DMEK uses no sutures. Routine activities resume in one to two weeks, but strenuous lifting is avoided for a month. Follow-ups occur at day 1, week 1, month 1, then every few months to monitor pressure and graft clarity.2 Mayo Clinic recommends lifelong annual exams because late rejection can occur even years after surgery.3
Latest Research & Innovations
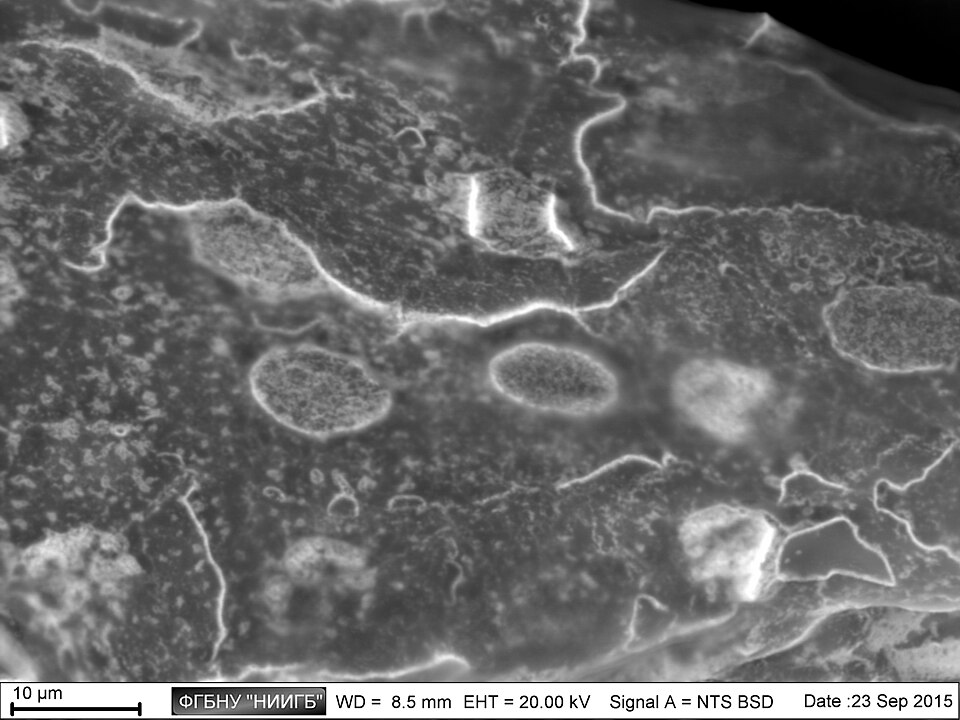
Surgeons are banking discarded lenticules from SMILE laser procedures as stroma on demand, and pilot trials of acellular bio-engineered corneas have restored sight in keratoconus. A 2024 review highlights endothelial cell therapy and gene-editing approaches that may one day replace donor tissue entirely.5 Ophthalmology Management reports ongoing U.S. trials of automated DMEK preparation and pre-loaded graft injectors that could streamline surgery and expand access worldwide.6
Recently Published in Peer-Reviewed Journals
Cornea
July 3, 2025
Quantifying Corneal Endothelial Cell Damage During Descemet Membrane Endothelial Keratoplasty Graft Loading and Ejection Using a Calcein-AM Imaging Method.
Lee S, Yuan C, Bedard P, et al.
Cornea
June 30, 2025
Tectonic Corneal Transplant in the Management of Congenital Anterior Staphyloma.
Rodrigues R, Scanga H, Potluri P, et al.
Cornea
June 3, 2025
Influence of Graft Donor Age in Descemet Membrane Endothelial Keratoplasty.
Wolf A, Della Volpe Waizel M, Darwisch W, et al.
Next Steps
If blurred vision, glare, or painful swelling limits your daily life, request a complete eye exam. A cornea specialist can measure corneal thickness, scan for dystrophies, and explain whether a full- or partial-thickness graft—or a non-surgical option—fits your needs. You can connect with the right specialist on Kerbside for a medical-education consult—no physician-patient relationship will be created.12
