Eyelid Twitch
Also known as Myokymia
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.
Overview
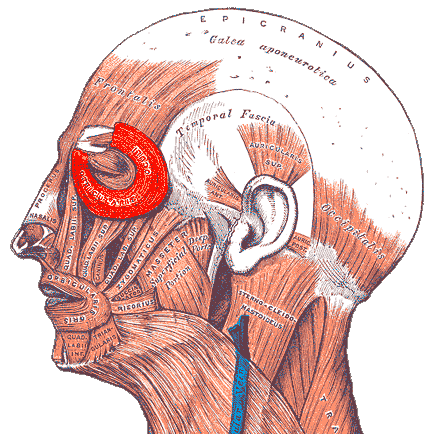
Eyelid twitch – the medical term is myokymia – is a sudden, repetitive spasm of the tiny muscle fibers that close the eyelid (the orbicularis oculi). It usually lasts seconds to minutes, disappears without treatment, and is considered benign in otherwise healthy eyes.1 Episodes often strike during times of fatigue, stress, or excess caffeine and may feel like a gentle flutter or ripple under the skin.2 Persistent twitching, twitching that involves other facial muscles, or spasms that force the lids shut can point to related movement disorders such as benign essential blepharospasm and deserve specialist review.3
Symptoms
Most twitches are barely noticeable; some feel strong enough to move the lashes. Typical features include:
- Brief, rhythmic contractions of the upper or lower lid, usually on one side.1
- Duration from a few seconds to several minutes – rarely hours.
- No pain or vision loss.
- Triggers: stress, lack of sleep, caffeine, dry eye, bright light, or prolonged screen use.5
Warning signs that warrant prompt evaluation include drooping eyelids, twitching spreading to the cheek or jaw, redness, discharge, or spasms that keep the eye closed.6
Causes and Risk Factors
An exact cause is often elusive, but well-recognized contributors include:
- Stress and fatigue – overstimulate facial nerve firing.2
- Caffeine, nicotine, or alcohol excess.
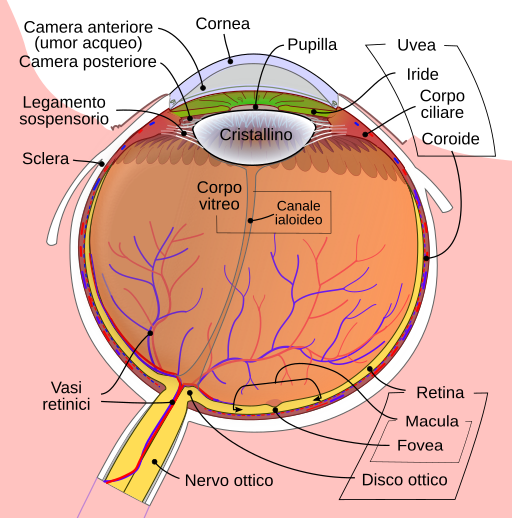
- Dry-eye or allergies that irritate the ocular surface.3
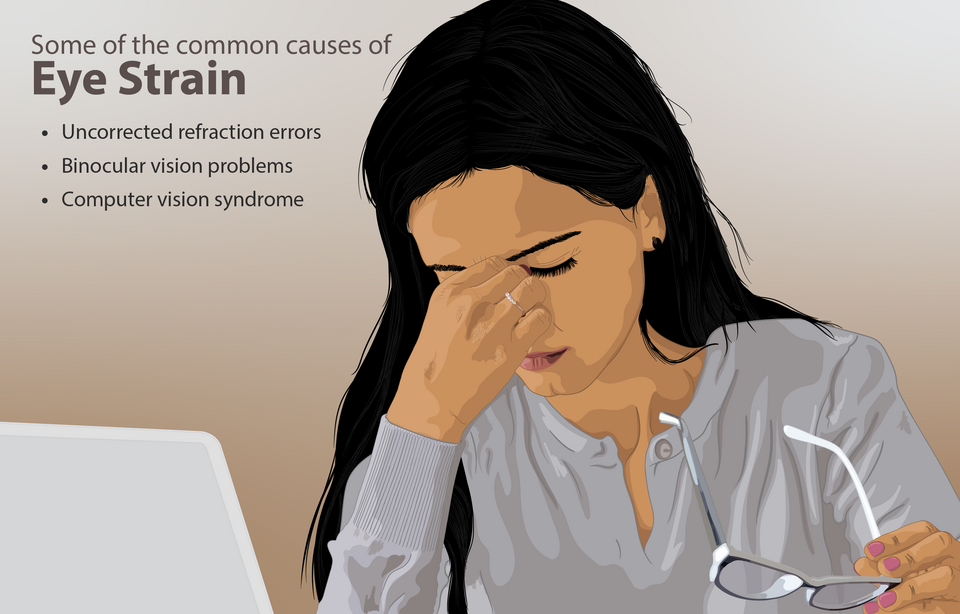
- Prolonged digital screen time leading to reduced blink rate and eye strain.5
- Medications (e.g., SSRIs, stimulants) or stimulatory eye drops.
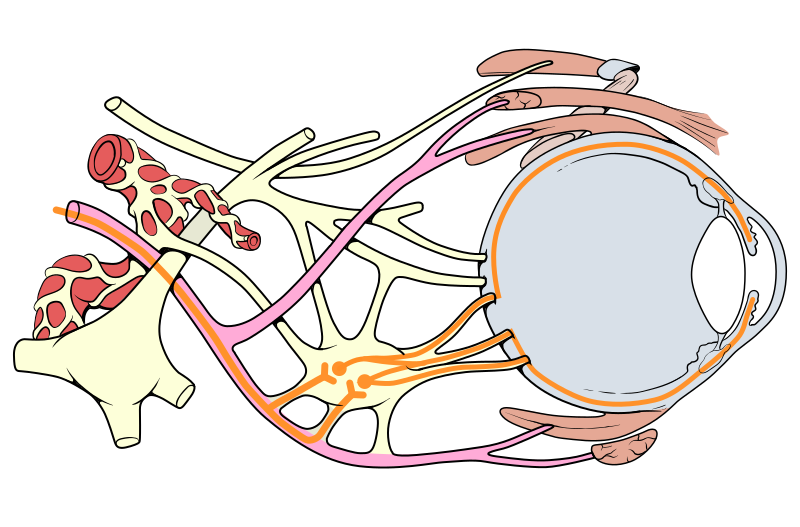
- Rare neurologic conditions such as multiple sclerosis, hemifacial spasm, or cranial nerve compression.4
Eyelid Twitch Risk Score
Select your details to estimate risk factors.
Diagnosis
Most cases are diagnosed in the exam room:
- History & inspection: The eye-care provider watches the twitch pattern and asks about triggers and systemic health.6
- Slit-lamp exam to rule out corneal irritation, dry eye, or foreign body.
- Neurologic screen for facial weakness or spasms.
- Imaging (MRI/CT) reserved for atypical, persistent, or hemifacial involvement suggesting nerve compression.3
Lab work is rarely needed unless systemic illnesses (thyroid, electrolyte imbalance) are suspected.4
Treatment and Management
For most people, simple lifestyle tweaks calm the eyelid:
- Sleep 7–8 hours nightly and incorporate stress-reduction practices like mindfulness or yoga.5
- Limit caffeine to ≤ 2 cups of coffee/cola per day.
- Apply warm compresses or gently massage the lids to relax the muscle fibers.2
- Lubricating eye drops if dryness or allergy is present.3
If twitching persists > 3 months or interferes with activities, office-based botulinum toxin injections can temporarily paralyze the over-active fibers and give relief for 3–4 months at a time.6 Rare underlying neurologic causes are treated by an ophthalmologist and, when needed, a neurologist.
Living with Eyelid Twitch and Prevention
You can keep twitches at bay with everyday habits:
- 20-20-20 rule: Every 20 minutes look 20 feet away for 20 seconds to reduce digital eye strain.5
- Hydrate and eat magnesium-rich foods (leafy greens, nuts) that support muscle relaxation.
- Quit smoking and moderate alcohol.
- Manage allergies with antihistamine drops to minimize ocular surface irritation.3
- Keep track of triggers in a journal and adjust lifestyle accordingly.
Because eyelid twitch is rarely dangerous, reassurance is important. Still, rapid access to care helps rule out rarer causes and provides peace of mind.1
Latest Research & Developments
Recent work is expanding what we know about myokymia:
- Digital-eye-strain studies show a direct correlation between uninterrupted screen time > 6 hours and transient eyelid spasms in office workers, strengthening prevention advice.7
- High-speed eyelid electromyography can now map abnormal firing patterns and predict which twitches will progress to blepharospasm.
- Long-acting botulinum formulations (daxibotulinumA) are in phase 3 trials aiming to double the treatment interval for chronic cases.
- Wearable blink-rate trackers are being tested to alert users when blink frequency drops during prolonged device use.
- Gene-association studies are exploring polymorphisms in calcium-channel genes as a potential predisposition to chronic myokymia.4
Recent Peer-Reviewed Research
Conversion of Superior Oblique Myokymia to Superior Oblique Neuromyotonia in a Patient With History of Superior Oblique Palsy.
Chen H, Subramanian PS
Disorders of the Fourth Cranial Nerve.
Kline LB, Demer JL, Vaphiades MS, et al.
William F. Hoyt and the Neuro-Ophthalmology of Superior Oblique Myokymia and Ocular Neuromyotonia.
Rasool N, Hoyt CS
Next Steps
If twitching lasts longer than two weeks, spreads to other facial muscles, or closes your eye, the best provider to consult is a neuro-ophthalmologist or oculoplastics specialist. They can distinguish simple myokymia from blepharospasm or hemifacial spasm and offer targeted therapy.
How to schedule: Start with your primary eye-care doctor; they may refer you urgently if red-flag signs are present. Many subspecialty clinics hold Botox days every 1–3 months for rapid treatment slots. Our Kerbside platform can connect you directly to board-certified subspecialists for second opinions or ongoing care without the usual wait times.
Trusted Specialists
Board-certified providers specializing in Eyelid Twitch.