Epithelial Basement Membrane Dystrophy
Last updated September 6, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.

Overview
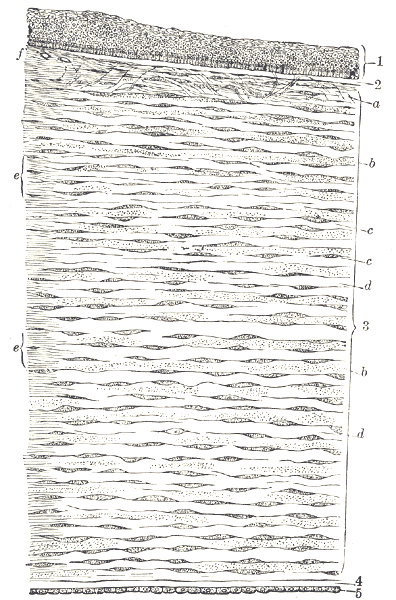
Epithelial basement membrane dystrophy (EBMD) is a common corneal condition in which the smooth surface cells (epithelium) do not adhere normally to the basement membrane. This can create map–dot–fingerprint patterns that blur vision or trigger painful recurrent corneal erosions. EBMD often affects both eyes and may wax and wane over time. 1
EBMD is most often found in adults, though it can appear earlier. Many people are asymptomatic and learn about it at routine exam. When symptoms occur, they relate to surface irregularity (blur/ghosting) or erosions (sudden pain, light sensitivity, tearing). 2
Symptoms
Symptoms range from mild/occasional to more frequent:
- Blurry or fluctuating vision, with glare/halos
- Ghosting or monocular double images
- Recurrent corneal erosions: sharp pain, tearing, photophobia—often on waking
- Foreign-body/gritty sensation
Some people have no symptoms, but the classic map–dot–fingerprint changes are seen on exam. 3
Causes and Risk Factors
In EBMD, an irregular/thickened basement membrane prevents normal epithelial anchoring, creating raised areas and tiny cysts (“dots”) and a fragile surface.
Risk clues:
- Age: more common in adults (often 40–70)
- Chronic surface irritation (dry eye, lid inflammation)
- Prior injuries or surgery disturbing the surface
- History of recurrent corneal erosions
Not everyone with these risks develops EBMD, and many with EBMD never have pain. 2 1
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
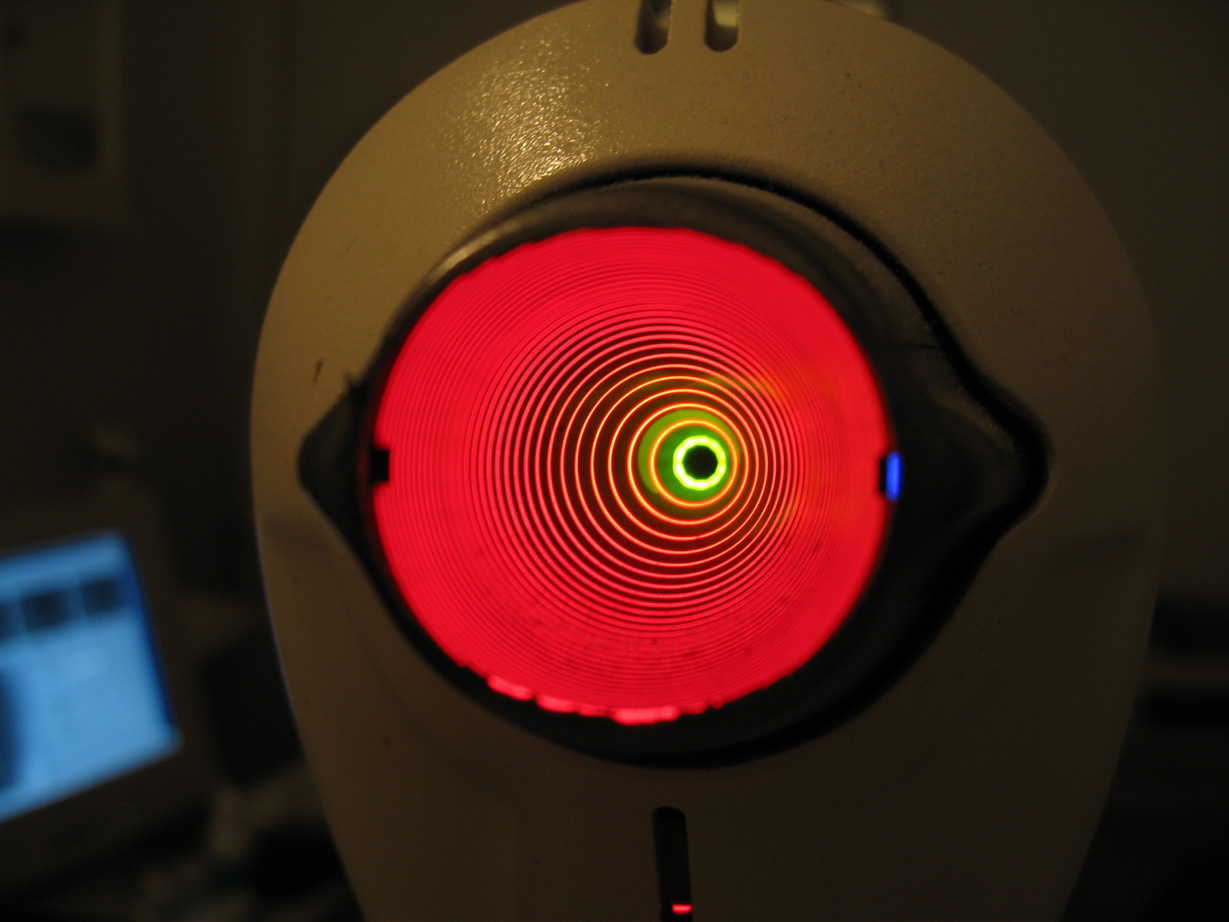
An eye doctor diagnoses EBMD at the slit lamp by identifying maps, dots, and fingerprint lines and assessing surface smoothness.
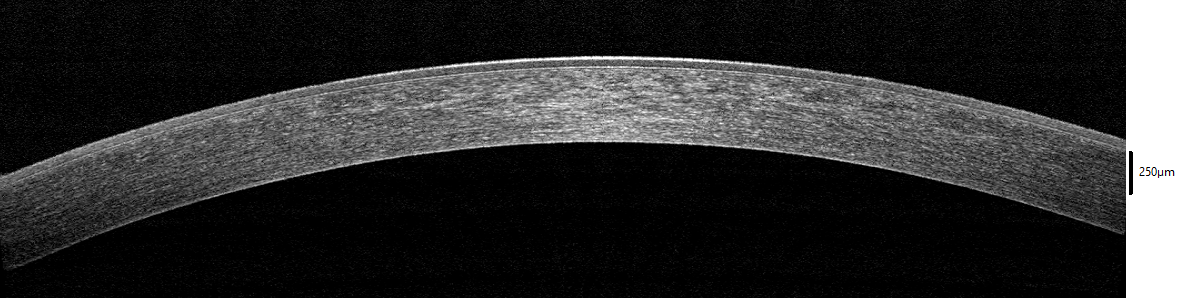
Helpful tests:
- Fluorescein dye with blue light to highlight rough or missing epithelium
- Corneal topography/tomography to map irregular astigmatism
- Anterior segment OCT to visualize layer changes and depth
These guide treatment and cataract planning because surface irregularity can alter measurements. 4 1
Treatment and Management
Care is tailored to symptoms—aiming to smooth the surface, reduce pain, and prevent erosions.
Home/medical (first steps):
- Artificial tears by day; thick ointment or hypertonic saline at bedtime to reduce morning sticking
- Lid hygiene and warm compresses for blocked oil glands
- Bandage soft contact lens short term during an erosion (with antibiotic drops and close follow-up)
- In select cases: doxycycline by mouth and a short topical steroid course to calm adhesion-worsening inflammation
Office procedures (if symptoms persist/vision reduced):
- Superficial keratectomy (SK) to remove loose/raised epithelium
- Diamond-burr polishing to smooth the base after SK
- Phototherapeutic keratectomy (PTK) for persistent irregularity or frequent erosions
Evidence for recurrent corneal erosions (often linked to EBMD) supports lubricants, bandage lenses, and—when needed—SK or PTK, individualized to the patient. 5 6
Living with EBMD and Prevention
Most people do well with steady care. Helpful habits:
- Nighttime protection: ointment or hypertonic saline before bed; upon waking, lubricate first, then open slowly
- Daytime moisture: use artificial tears; consider a humidifier and screen breaks
- Avoid eye rubbing
- Manage dryness and lids: treat dry eye/blepharitis
- Plan around surgeries: optimize the surface before cataract measurements
Regular exams and good surface care reduce erosions and stabilize vision. 2
Latest Research & Developments
Cataract planning: EBMD can distort pre-op biometry/keratometry; treating the surface (e.g., SK/PTK) first may improve accuracy and outcomes. 7
Laser smoothing (PTK): Studies report improved vision and fewer erosions in selected EBMD patients when medical care is insufficient; long-term follow-up tracks vision, comfort, and recurrence. 8
Recently Published in Peer-Reviewed Journals
Cornea
August 1, 2024
Pilot Safety Study of a Microfabricated Device for Anterior Stromal Puncture to Treat Corneal Epithelial Disease in the Optical Axis.
Chaum E, Kim DB, Kane S, et al.
Cornea
August 1, 2023
Anterior Segment Swept Source Optical Coherence Tomography and In Vivo Confocal Microscopy Findings in a Case With Bleb-Like Epithelial Basal Membrane Dystrophy.
Eker S, Oflaz AB, Bozkurt B
Cornea
August 1, 2022
Bowman Layer Onlay Graft for Recurrent Corneal Erosions in Map-Dot-Fingerprint Dystrophy.
Mulders-Al-Saady R, van der Star L, van Dijk K, et al.
Next Steps
If you have EBMD symptoms or recurrent erosions, see a cornea specialist (ophthalmologist). Many start with an optometrist/general ophthalmologist and are referred if symptoms persist.
- How to schedule: request a “cornea evaluation for EBMD or recurrent corneal erosion”; bring glasses/contacts info, drop list, and prior records; obtain referral if required
- What to expect: topography (surface mapping), OCT imaging, and a slit-lamp exam; treatment usually begins with lubrication and escalates only if needed
- Educational help: Kerbside can help you prepare (informational only; not a patient–physician relationship)
