Recurrent Corneal Erosion
Also known as Recurrent Erosion Syndrome
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
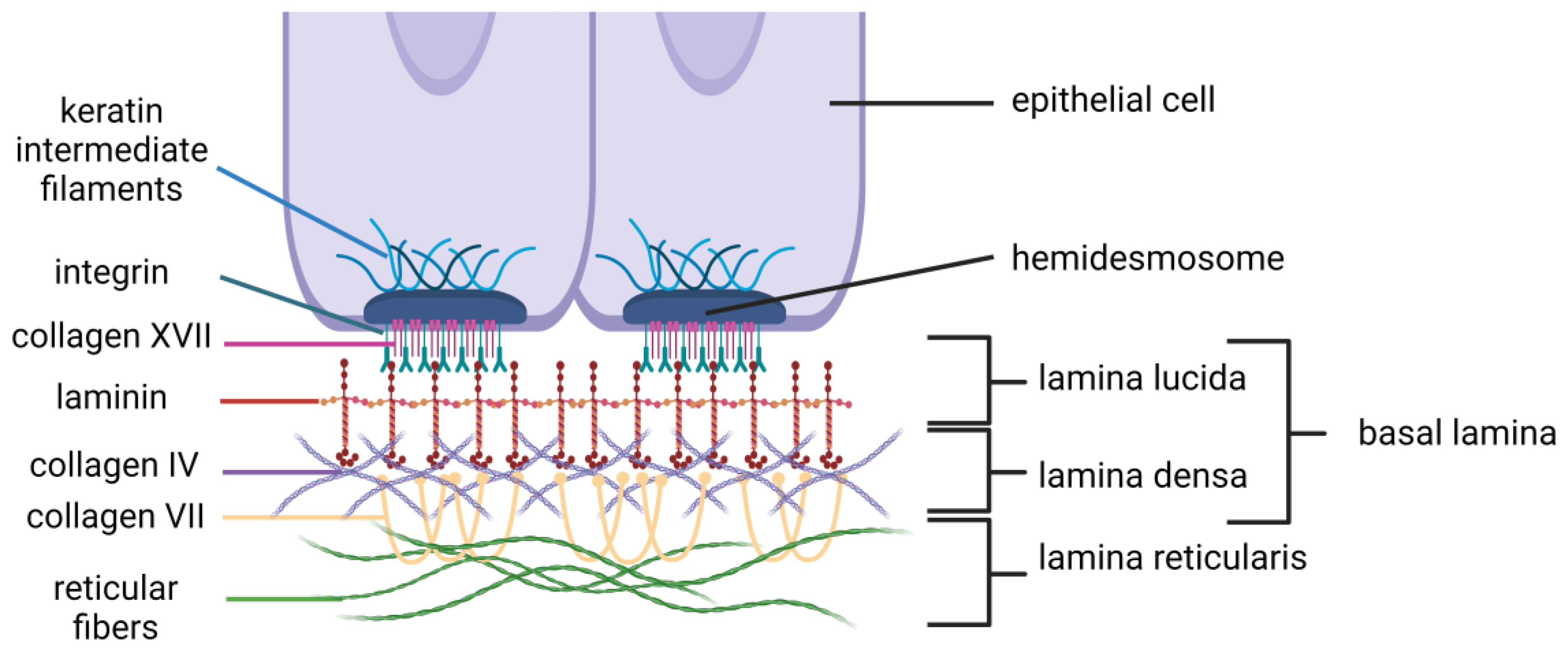
Recurrent corneal erosion (RCE) occurs when the corneal surface (epithelium) does not firmly adhere to the layer beneath it. The surface can lift or tear repeatedly, causing sudden pain, tearing, light sensitivity, and blurry vision—often right after waking. Many people first develop RCE after a scratch; others have an underlying corneal condition that makes the surface cells fragile. 1
RCE is treatable. Most people do well with a plan combining lubrication, protection while the surface heals, and—when needed—office procedures that improve adhesion. 2
Symptoms
RCE symptoms can come and go and may affect one or both eyes. Common symptoms include:
- Sharp eye pain, often on first opening the eye in the morning
- Watering and light sensitivity (photophobia)
- Blurry vision or a gritty, sandy feeling
- Redness and trouble keeping the eye open
Attacks can last minutes to hours and may be frequent small episodes or rare severe ones. If these symptoms occur, seek an eye evaluation. 2
Causes and Risk Factors
RCE usually starts in one of two ways:
- After a corneal scratch (abrasion): The healed surface may not fully reconnect to the underlying layer, so it can peel up again later.
- Because of a corneal condition: The most common is epithelial basement membrane dystrophy (EBMD), also called map–dot–fingerprint dystrophy, which weakens adhesion. 4
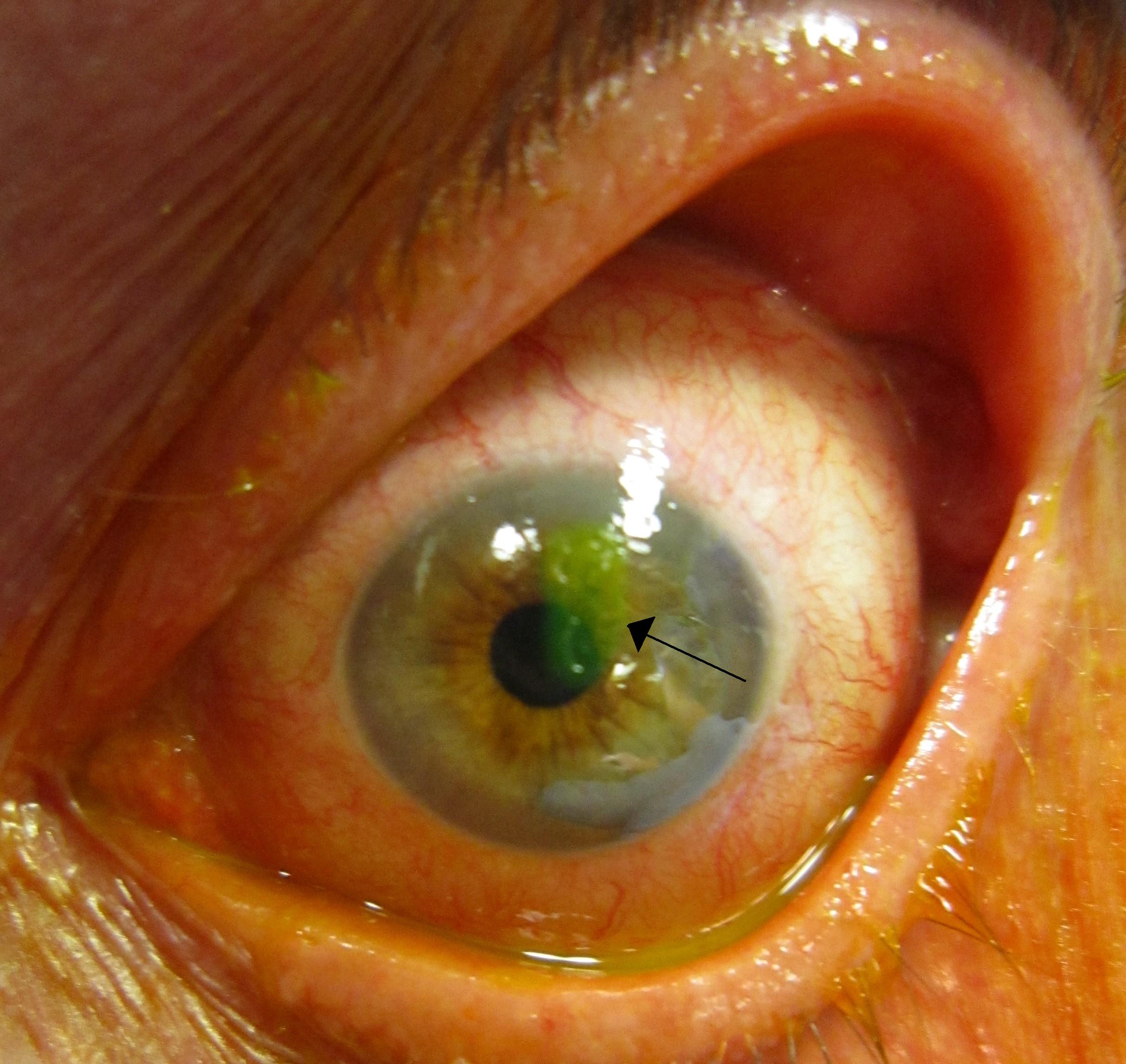
Other risk clues include dry eye, eye rubbing, sleeping with eyes slightly open, diabetes, and previous eye surgery or trauma. Tiny negative-staining patterns with fluorescein dye can suggest loose surface cells. 1
RCE 1-Year Recurrence Risk (Simple Score, Assumption-Based)
Select your details to estimate risk factors.
Diagnosis
An eye doctor (optometrist or ophthalmologist) makes the diagnosis after a slit-lamp exam. They may:
- Instill fluorescein dye and examine with blue light for missing/uneven surface or negative staining
- Check vision and corneal sensitivity
- Look for signs of EBMD or other weakening conditions
- Review history of injury, dry eye, or nighttime symptoms
Sometimes corneal OCT helps map thin or irregular areas. The combination of a typical history (morning pain like a fresh scratch) plus exam usually confirms RCE. 1 2
Treatment and Management
Goals are to help the epithelium heal firmly and stay attached. Treatment is tailored to flare frequency and severity.
First-line care (often at home):
- Lubrication: artificial tears by day; thick ointment at bedtime
- Hypertonic saline (e.g., 5% drops/ointment) at night to reduce overnight swelling
- Antibiotic ointment for a few days if an open area is present
- Pain control with cold compresses and oral medicine as advised
Office therapies if episodes keep returning:
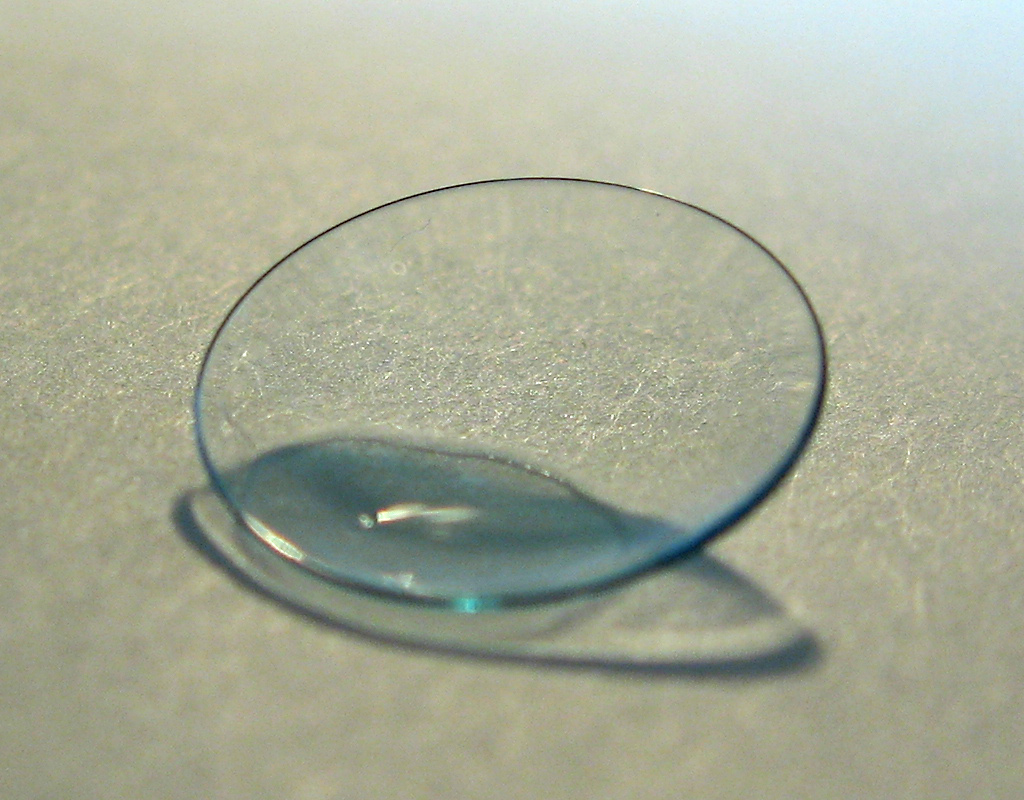
- Bandage soft contact lens (with antibiotic drops and close follow-up)
- Doxycycline by mouth plus a short topical steroid course (when appropriate)
- Anterior stromal puncture (tiny, controlled pokes outside the visual center)
- Diamond-burr polishing or epithelial debridement to remove loose cells
- Phototherapeutic keratectomy (PTK) for persistent cases
Your doctor will choose the least invasive option that fits your cornea and lifestyle. With a steady plan, most people improve and attacks become rare. 1 3
Living with Recurrent Corneal Erosion and Prevention
Daily habits can lower the chance of another episode:
- Nighttime routine: Use ointment or hypertonic saline before bed; on waking, lubricate first and then open eyes slowly.
- Surface protection: Avoid rubbing; use a humidifier if air is dry; ask about a nighttime shield or gentle lid taping if lids don’t seal well.
- Manage triggers: Treat dry eye, allergies, and eyelid problems; consider sleep apnea screening if you wake with dryness.
- Safety: Wear protective eyewear for sports/yardwork; if a new scratch happens, seek care early.
With consistent care, most people keep good vision and see fewer, milder flares over time. 2
Latest Research & Developments
What works best? A Cochrane review found that common options—bandage lenses, anterior stromal puncture, diamond-burr polishing, and PTK—can help; the best choice depends on the individual and erosion location. More high-quality trials are needed to rank treatments clearly. 3
Link with EBMD and dry eye: Ongoing work explores how EBMD and surface dryness raise recurrence risk and how steroids, doxycycline, and advanced lubricants may improve adhesion. Micro-procedures and laser PTK remain important for stubborn cases. 1
Recent Peer-Reviewed Research
Atypical Migratory Serpiginous Corneal Epitheliopathy: Unmasking Herpes Simplex Virus Association.
Shields C, Buggareddigari S, Jakati S, et al.
A comparative analysis of the 1-year outcomes of modified Athens protocol versus Cretan protocol in the treatment of progressive keratoconus.
Huang J, Wu J, Xiao W, et al.
Safety and Efficacy of Corneal Crosslinking Combined With Phototherapeutic Keratectomy With or Without Topography-Guided Photorefractive Keratectomy.
Gil P, Gil JQ, Dias M, et al.
Next Steps
If you think you have RCE or just had a new episode, see a cornea specialist (ophthalmologist). Many start with an optometrist or comprehensive ophthalmologist and are referred if flares continue.
- How to schedule: Ask for a “recurrent corneal erosion evaluation.” Bring glasses/contacts info, a list of drops, and prior eye records. Get an insurance referral if required.
- Timing tips: Request the cancellation list. Mention that mornings are worst—clinics may try to see you early.
- Educational help: Kerbside can provide a medical education consult to prepare for your visit (educational only; no physician–patient relationship).