Episcleritis
Last updated August 31, 2025
Medical information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis or treatment.
See our Terms & Conditions and Consent for Telemedicine for details.


Overview
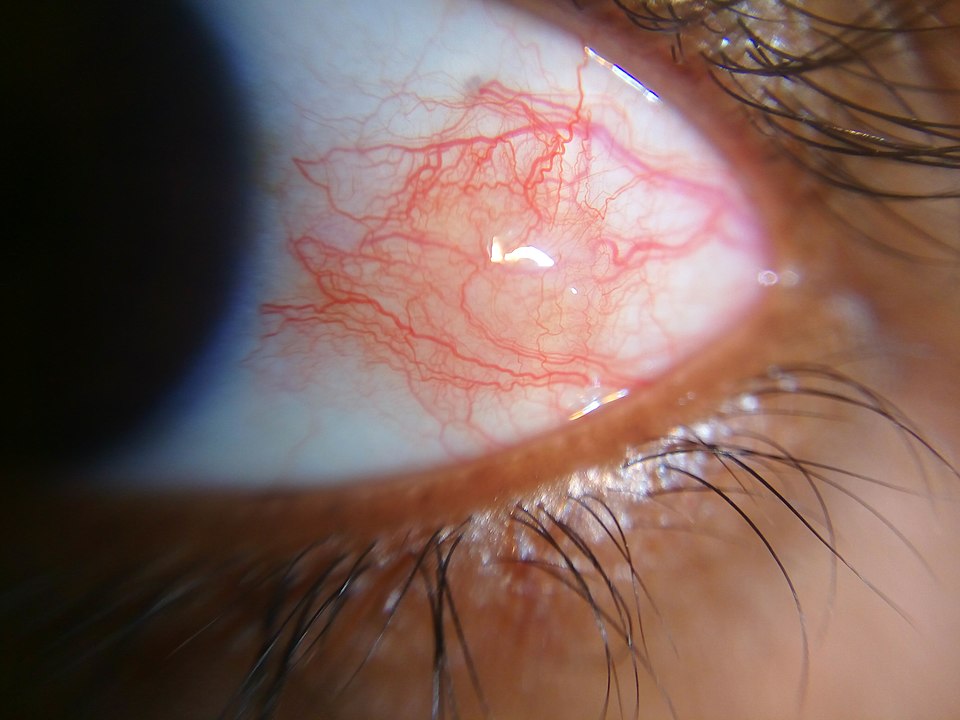
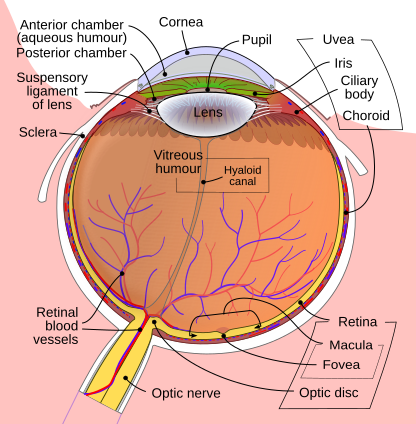
Episcleritis is a short-lived inflammation of the thin, stretchy layer over the white of the eye (the episclera). It often shows as a bright red or pink patch in one eye, with mild tenderness or irritation but usually little to no pain or vision loss. Most episodes clear on their own in a few weeks. 1
Doctors describe two main patterns: simple episcleritis (diffuse or sectoral redness) and nodular episcleritis (a small, tender raised spot). Some people have repeat flares, and a minority have an underlying autoimmune condition, so an eye exam is important—especially for first-time or recurrent cases. 2
Symptoms
The key sign is sectoral redness—a wedge or patch of red on the white of the eye. Many people describe mild soreness, a gritty feeling, tearing, and light sensitivity. Vision is usually normal, and discharge is uncommon. 3 Symptoms can rise quickly, often peaking within ~12 hours, then fade over days as inflammation settles.
Common clues:
- Tender spot to touch
- Redness that looks “flat” on the surface
- Mild light sensitivity and watery eyes
Less common: a small raised nodule (nodular episcleritis) that is more tender than the simple form.
Get same-day care if redness comes with severe pain, worsening light sensitivity, or sudden blur—these are red flags for other conditions. 4
Causes and Risk Factors
Most cases are idiopathic (no exact cause found). When a cause exists, common links include autoimmune/connective tissue diseases (rheumatoid arthritis, lupus, psoriatic arthritis, inflammatory bowel disease). Skin conditions like rosacea can also be associated. 1
Less often, infections such as herpes zoster, syphilis, tuberculosis, or Lyme disease may trigger inflammation. Women are affected more often, episodes typically begin in early–mid adulthood, and recurrences are common but usually mild. 2
Flares may follow stress, seasonal allergies, hormonal shifts, or eye irritation (not proven causes). If you have an autoimmune diagnosis, keeping it well controlled can reduce eye inflammation and shorten recovery time.
Episcleritis Risk Checker
Enter your details in the following fields to calculate your risk
Risk Level
Recommendation
Diagnosis
An eye-care professional confirms the diagnosis with a slit-lamp exam. One helpful in-office check is the phenylephrine blanching test: a drop of dilute phenylephrine temporarily shrinks superficial blood vessels. If redness eases after the drop, episcleritis is likely; if it does not blanch, deeper inflammation like scleritis is suspected and needs urgent attention. 2
The doctor also looks for a tender nodule, checks for light sensitivity, and ensures the cornea and inside of the eye are quiet—findings that help separate episcleritis from more serious causes of a red eye. 3
Blood tests are not routine for a first simple episode. For recurrent or nodular cases, targeted labs or a rheumatology workup may be recommended to uncover an associated systemic condition.
Treatment and Management
Episcleritis often settles without treatment. Care focuses on comfort and calming inflammation while ruling out more serious problems.
Self-care:
- Preservative-free artificial tears several times daily
- Cool compresses for a few minutes at a time
- Sunglasses to reduce wind and bright light
Medicines: If symptoms are bothersome, doctors may suggest an oral NSAID (e.g., ibuprofen, if safe for you) or a short course of a mild topical steroid drop. These can speed comfort but require monitoring to avoid side effects like eye pressure rise. 3
Underlying conditions: Working with your primary team/rheumatologist to control autoimmune disease can reduce eye flares and recurrences.
Most people improve over 2–3 weeks, often sooner with supportive care. Your eye doctor will tailor drops, check eye pressure if steroids are used, and guide a slow taper to prevent rebound redness. 1
Living with Episcleritis and Prevention
You can usually continue normal activities during a flare, with a few tweaks to reduce irritation:
- Screen-time breaks: 20–20–20 rule; use lubricating drops as needed.
- Light & wind: Sunglasses or light tints outdoors; consider wraparound frames.
- Allergy & dryness: Manage with your clinician’s guidance.
- Healthy routines: Sleep, stress reduction, and control of autoimmune disease.
Call an eye doctor the same day for severe pain, sudden vision changes, marked light sensitivity, or if redness is not improving—these may signal a different and more serious problem. 4 Most people with episcleritis recover fully and learn to spot early signs and treat discomfort quickly with safe, simple steps. 1
Latest Research & Developments
Newer imaging helps distinguish episcleritis from scleritis and track healing. Anterior segment OCT (AS-OCT) can measure tissue changes and show where inflammation sits—superficial in episcleritis vs. deeper in scleritis—supporting faster, safer decisions. 5
Studies also report that AS-OCT can visualize scleral thickening and edema during active disease and document improvement with treatment, offering an objective way to monitor response over time. 6
Recently Published in Peer-Reviewed Journals
American journal of ophthalmology
August 1, 2025
Ocular Features of VEXAS Syndrome: A Systematic Review and Meta-analysis.
Quigley C, Pietris J, Ang T, et al.
Eye (London, England)
June 1, 2024
Ocular and orbital manifestations in VEXAS syndrome.
Abumanhal M, Leibovitch I, Zisapel M, et al.
BMC ophthalmology
January 18, 2023
The eye is a common site of granulomatosis with polyangiitis. A collaborative study.
Dammacco R, Biswas J, Mohanan-Earatt A, et al.
Next Steps
If you develop a new, bright red patch on the white of your eye—especially with tenderness—book an exam with an ophthalmologist (preferably with uveitis/ocular inflammation expertise). Tell the scheduler you have “possible episcleritis” and ask about urgent/cancellation slots. Bring a list of symptoms, timing, and any autoimmune diagnoses or medicines. 3
After the exam, follow the plan for drops, cool compresses, and follow-up so your doctor can confirm healing and adjust therapy. You can also connect on Kerbside for a medical education consult with the right specialist (no patient–physician relationship is established).