Demodex Blepharitis
Also known as Eyelash Mite Blepharitis
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.



Overview
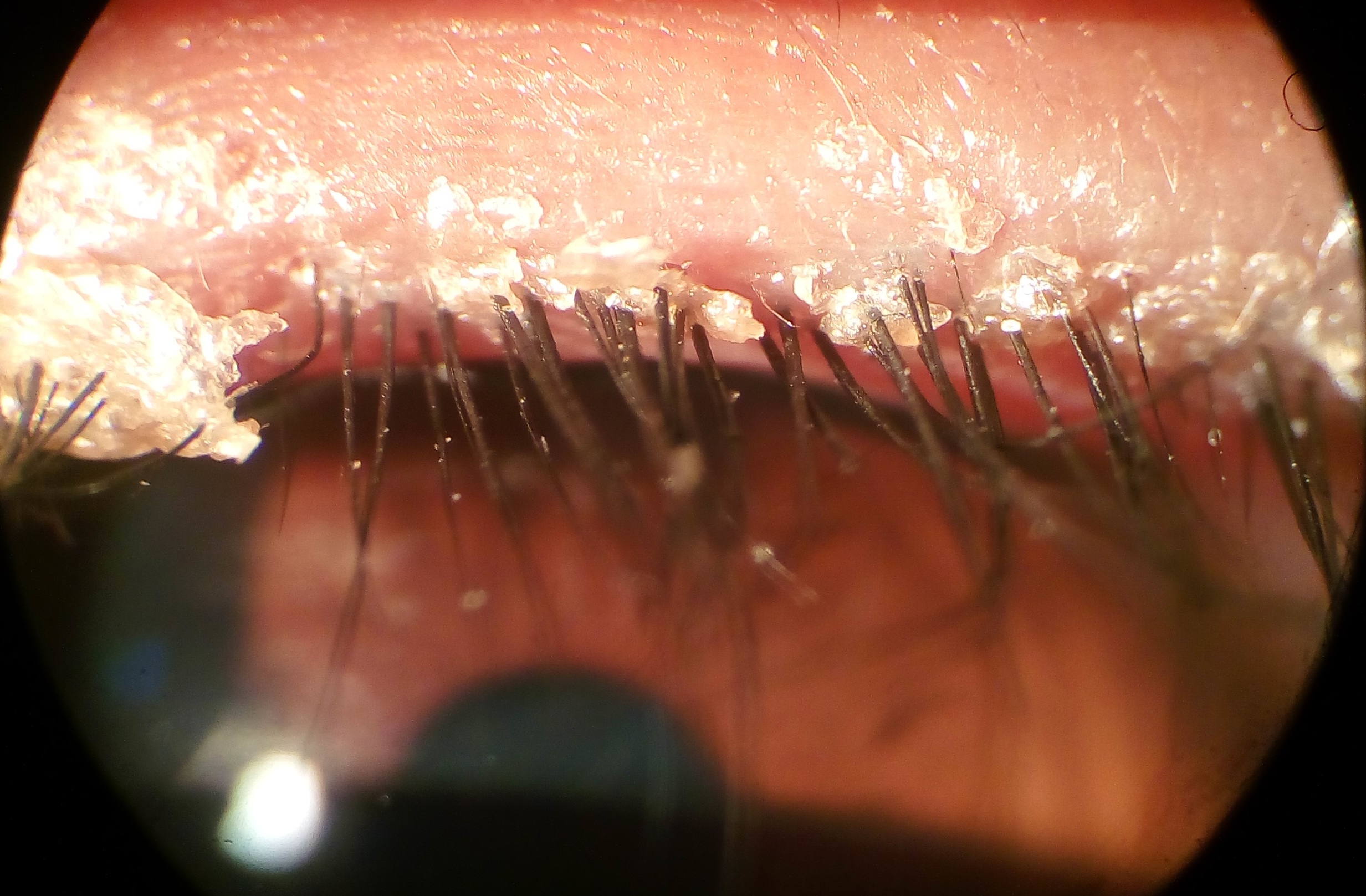
Demodex blepharitis is eyelid inflammation caused by an overgrowth of tiny mites (Demodex) that live in hair follicles and oil glands. Many people have a few mites and feel fine, but too many can irritate the eyelids and lashes. A key sign is collarettes—waxy sleeves around the base of eyelashes. Doctors also look for redness, itching, and crusting along the lid margin. 1
- Collarettes are considered the hallmark of Demodex blepharitis and are common in eye clinics, so the condition is often underdiagnosed unless the lashes are checked closely. 2
Symptoms
Symptoms can be mild at first and may come and go. They often include:
- Itchy, irritated lids—especially along the lash line.
- Redness, burning, or gritty sensation (like something is in the eye).
- Crusting or flakes stuck to the lashes (collarettes).
- Watery or dry eyes, light sensitivity, or blurry vision that improves with blinking.
Because symptoms overlap with other lid problems, regular eye exams help confirm what’s going on and guide treatment. 3 If you have frequent styes or chalazia (lid bumps), Demodex may be part of the picture. 4
Causes and Risk Factors
Two mite species—Demodex folliculorum (lives in lash follicles) and Demodex brevis (lives in oil glands)—can overgrow and inflame the eyelids. Collarettes form from shed skin, oils, and mite waste at the lash base. 5 The main risk is simple: more mites than your lids can tolerate.
- Age (mites become more common with age).
- Oily skin, rosacea, or meibomian gland dysfunction.
- Contact lens wear or heavy eye makeup that isn’t fully removed.
- Chronic lid disease or prior untreated blepharitis.
Not everyone with mites has symptoms, but when collarettes appear with irritation, Demodex blepharitis is likely. 1
Demodex Blepharitis: Simple 6-Month Flare Risk (Assumption-Based)
Select your details to estimate risk factors.
Diagnosis
A trained eye care professional can diagnose Demodex blepharitis at the slit lamp. Steps usually include:
- Looking-down test: you look down so the doctor can inspect the base of the upper lashes for collarettes (telltale sleeves).
- Lid margin exam for redness, plugged oil glands, or scaly skin.
- Ocular surface check for dryness or corneal staining.
- Sometimes a few lashes are gently removed and examined under a microscope, but this is not always needed when collarettes are clearly present.
Clinical guidance supports using collarettes as the key sign to make the diagnosis and start care. 5 Cylindrical dandruff around lashes is also described in blepharitis references. 6
Treatment and Management
Goal: reduce mites, calm inflammation, and keep lids clean. Your doctor will tailor a plan. Common tools include:
- Lid hygiene: Warm compresses and gentle lid scrubs to remove debris; your clinician may recommend a cleanser safe for lids.
- Prescription therapy (lotilaner 0.25%): The first FDA-approved eye drop for Demodex blepharitis (XDEMVY), used twice daily for 6 weeks. In clinical studies it reduced collarettes and mites and improved eyelid redness. A randomized controlled trial showed lotilaner was superior to vehicle in clearing collarettes and reducing mite counts. 8
- Other supportive care: Artificial tears, short courses of anti-inflammatory drops if the eye surface is irritated, and treatment of related problems like MGD or rosacea.
How long? Many people feel and see improvement over several weeks; your doctor will re-check after a treatment cycle and may advise maintenance hygiene to lower recurrence. 7
Costs & price (practical tips)
- Prescription drops: Ask if your plan covers lotilaner and whether prior authorization is needed; notes about collarettes and symptoms can help.
- Pharmacy shopping: Prices vary; some manufacturers offer copay support for eligible patients.
- Visits & testing: Expect an initial exam and a follow-up after treatment; request a pre-estimate for any extra dry eye/MGD testing.
- Budget-friendly habits: Keep warm compresses and daily lid hygiene long term to reduce flares.
Living with Demodex Blepharitis and Prevention
Most people do well with steady care. Daily habits that help:
- Clean lids every day as directed—especially after makeup use.
- Replace or clean eye makeup tools regularly; avoid sharing them.
- Manage skin conditions (e.g., rosacea) with your dermatologist.
- Follow contact lens hygiene; consider lens breaks during flares.
- Call if symptoms return: recurrent collarettes or itching may need another treatment cycle.
Routine eyelid care lowers the chance of flares and can improve comfort and vision in everyday activities. 3
Latest Research & Developments
There is active research on better ways to identify and treat Demodex blepharitis. The FDA recognized lotilaner 0.25% as the first drug specifically approved for this condition, based on two pivotal trials. 9 Peer-reviewed studies continue to report improvements in collarette clearance, mite reduction, and eyelid redness with lotilaner in hundreds of patients. 10 Experts have also published consensus guidance to standardize diagnosis (look for collarettes at lash bases) and align treatment steps with severity. 5
Recent Peer-Reviewed Research
Identification of tear lipid biomarkers in women with dry eye disease and the impact of intense pulsed light therapy: a case-control study.
Acera A, Ibarrondo O, Mateo-Orobia AJ, et al.
Letter Regarding "Investigating Risk Factors for Meibomian Gland Dysfunction and Loss Among Young Medical Trainees".
Tripathi M, Markan A
Factors Associated With Perfluorohexyloctane Treatment Response in Dry Eye Disease Associated With Meibomian Gland Dysfunction.
Gu H, Li Z, Zhu L
Next Steps
If you think you have Demodex blepharitis—or were just diagnosed—the best clinician to see is an ophthalmologist (glaucoma or cornea/external disease) or an optometrist experienced in lid disease. Many primary eye doctors manage this; referral is considered if severe or recurrent.
- How to schedule: Ask for a “blepharitis evaluation.” Bring your medications, eye makeup/lens routines, and any photos of lid crusting. If your insurance needs a referral, call primary care first.
- Timing tips: Request the cancellation list; new swelling, pain, or vision drop should be seen sooner.
- Extra help: You can connect with a specialist on Kerbside for a medical education consult (educational only; no physician–patient relationship).
Trusted Specialists
Board-certified providers specializing in Demodex Blepharitis.
