Acanthamoeba Keratitis
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.
Overview
Acanthamoeba keratitis (AK) is a rare but serious infection of the clear front surface of the eye (cornea) caused by a tiny organism found in water, soil, and dust. It most often affects people who wear contact lenses, especially when lenses are exposed to water. AK can cause severe pain and vision loss if not treated quickly, so any new, painful red eye—particularly in a contact lens wearer—should be evaluated by an eye specialist right away. Early diagnosis and treatment can protect sight, but recovery is often slow. 1 The condition can mimic more common infections at first, which is why a high level of suspicion is important when symptoms don’t improve as expected. 2
Symptoms
People with AK usually notice significant pain that can seem worse than the early exam findings. Other symptoms include eye redness, tearing, light sensitivity, blurry vision, and the feeling of something in the eye. Symptoms may begin gradually and can last for weeks if untreated. Contact lens wearers are most often affected, but anyone can get AK if the cornea is exposed to contaminated water or soil. 1
Eye doctors look for features such as a ring-shaped corneal infiltrate (a circular area of inflammation) and perineural infiltrates (inflammation along corneal nerves). Because early AK resembles bacterial, viral, or fungal keratitis, misdiagnosis is common and can delay appropriate therapy. 3
Causes and Risk Factors
Acanthamoeba are free-living microbes found worldwide in water (including tap water), soil, and dust. Most cases of AK occur in contact lens users. Risk rises with behaviors that bring lenses into contact with water, such as swimming, showering, or using a hot tub while wearing lenses, or rinsing/soaking lenses or cases with water or homemade solutions. 4
Why is this infection hard to treat? Acanthamoeba can form a tough, protective cyst that survives harsh conditions and resists many disinfectants. This, along with variable early signs, contributes to underdiagnosis and challenging treatment courses. 8 While most patients are lens wearers, non–lens wearers can develop AK after corneal injury or exposure to contaminated water or soil.
AK Urgency & Likelihood Score (for painful red eye in contact lens wearers)
Select your details to estimate risk factors.
Diagnosis
AK is diagnosed by combining the exam with specialized tests. Your eye doctor will take a careful history (including contact lens care and any water exposure), check vision, and examine the cornea with a slit lamp. Classic clues include a ring-shaped infiltrate and inflammation along corneal nerves ("radial keratoneuritis"). 2
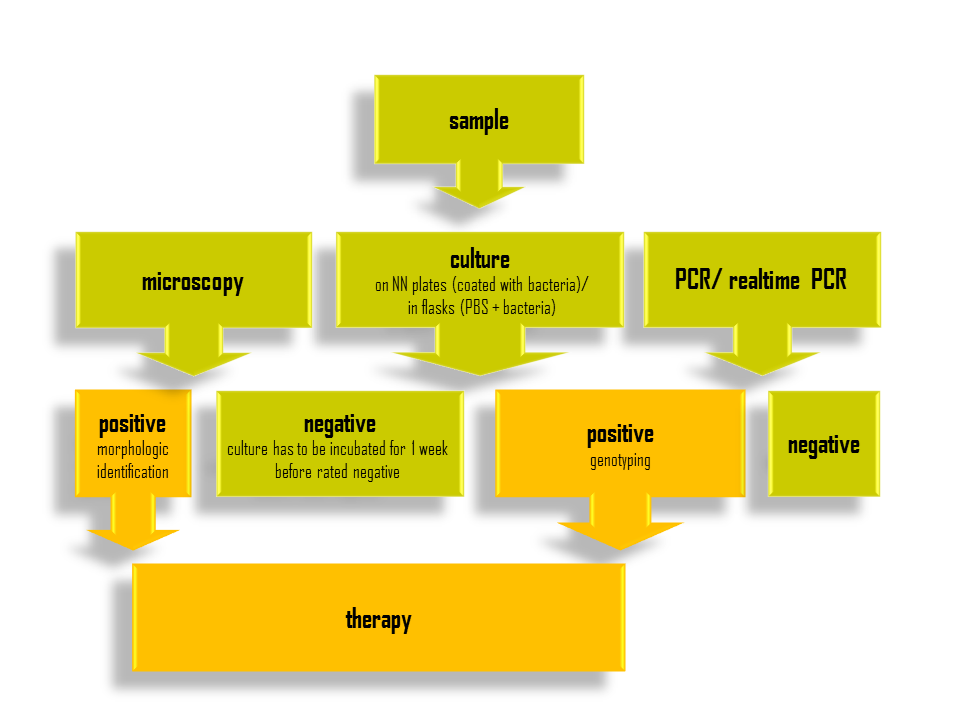
To confirm the diagnosis, doctors may perform one or more of these tests:
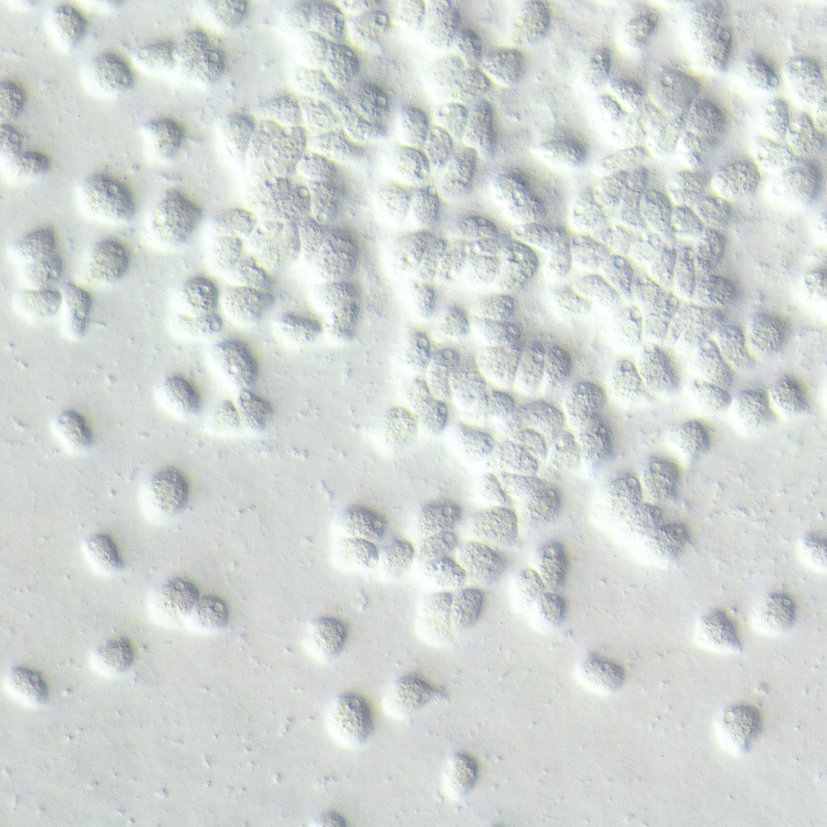
- Corneal scraping/culture: a small sample is placed on non-nutrient agar with bacteria to encourage Acanthamoeba growth.
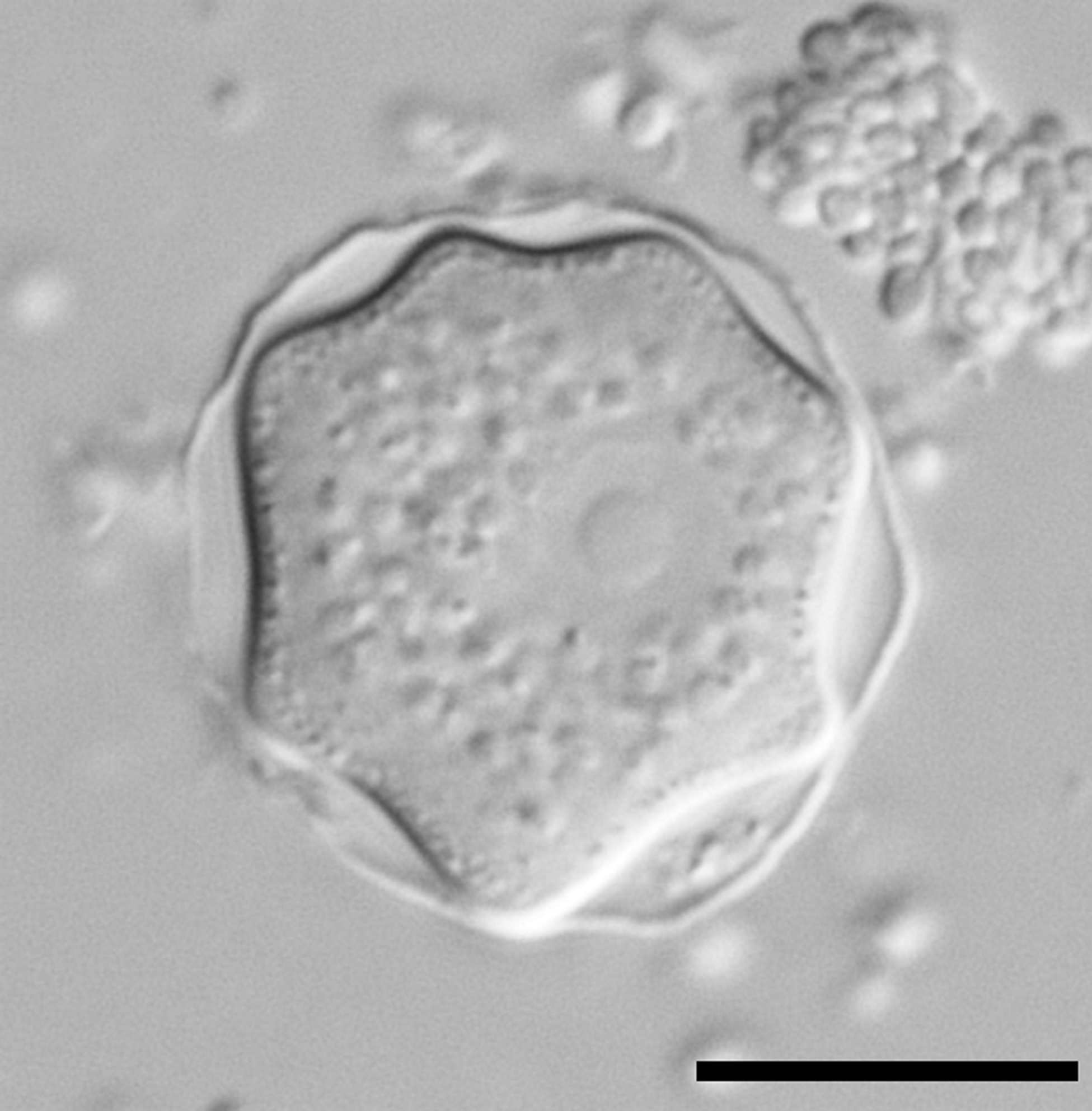
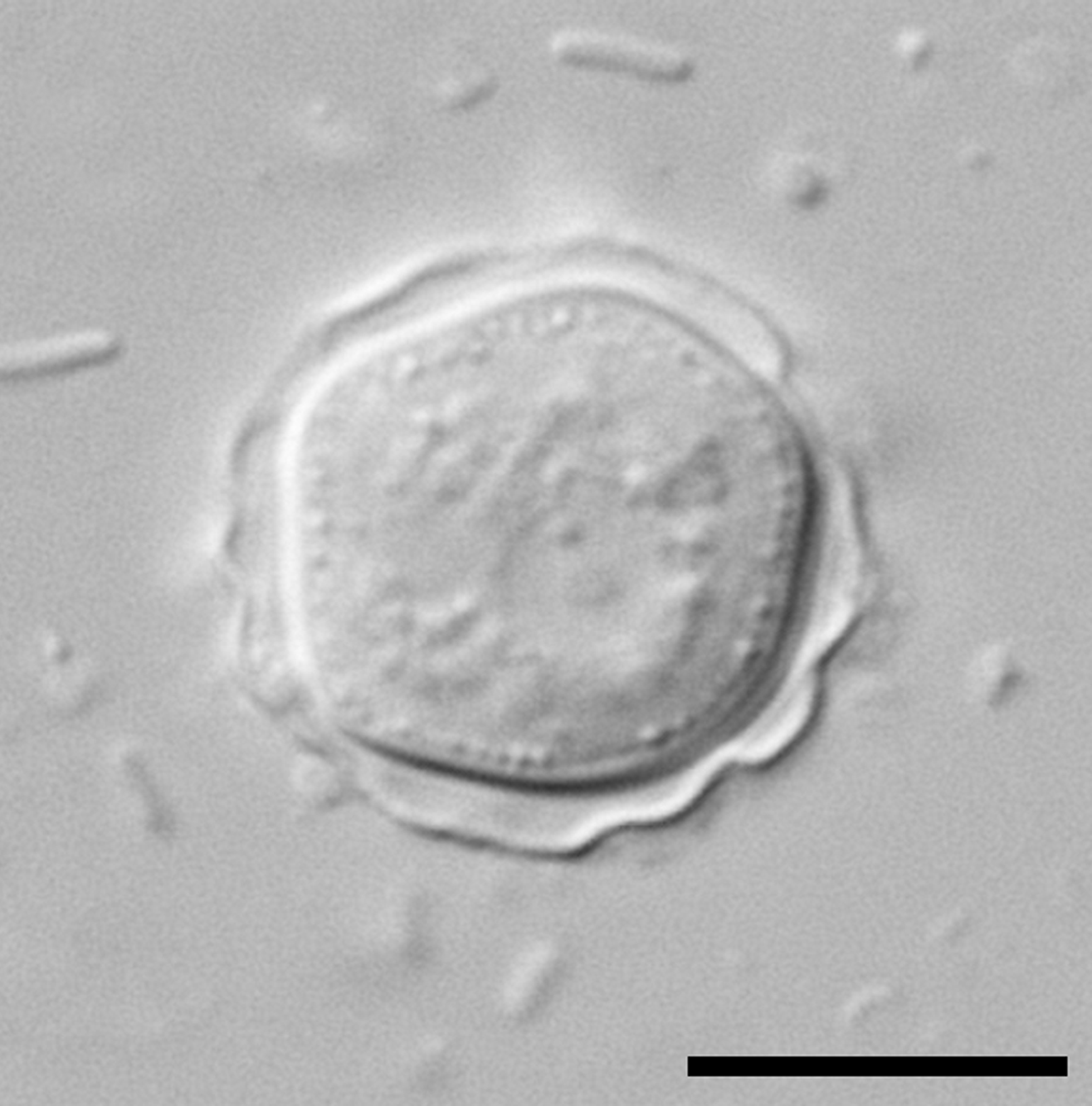
- In vivo confocal microscopy: a noninvasive scan that can show double-walled cysts within the cornea, supporting AK when seen with typical signs.
- PCR testing: detects Acanthamoeba DNA and may provide faster answers than culture.
Because AK is uncommon and can look like other infections, expert guidance encourages early consideration of AK in contact lens wearers with severe pain or poor response to initial treatment. 7
Treatment and Management
Treatment focuses on killing both the active forms (trophozoites) and the hardy cysts. Therapy often starts as soon as AK is suspected, because delays may worsen outcomes. Most patients need frequent anti-amoebic eye drops for weeks to months and close follow-up.
- First-line medicines: topical biguanides such as polyhexamethylene biguanide (PHMB) 0.02% or chlorhexidine 0.02%, often combined with a diamidine like propamidine 0.1% or hexamidine. Treatment is typically hourly at first, then gradually tapered as the eye improves.
- Newer options and evolving evidence: Recent clinical research suggests PHMB 0.08% monotherapy may achieve cure rates comparable to combination regimens when used with a standardized protocol. 9
- Steroid use: Topical steroids can sometimes worsen infection if started too early; they may be used cautiously later to control inflammation when the infection is under control—this decision is individualized by your specialist.
- Adjuncts and surgery: For resistant cases, doctors may consider additional agents (for example, miltefosine as an adjunct in some reports) or procedures. Severe scarring, thinning, or perforation may require a corneal transplant to restore the eye’s structure and vision. 6
Even with correct therapy, healing can be slow. Your care plan will include pain control, stopping contact lens wear, and frequent check-ins to adjust treatment.
Living with Acanthamoeba Keratitis and Prevention
AK can be physically and emotionally challenging. Many people need months of treatment and several follow-up visits. It’s normal to feel frustrated or worried during recovery. Staying consistent with drops, keeping your appointments, and asking questions can make a big difference. If your pain suddenly worsens or vision declines, contact your eye team urgently.
Prevention tips (especially for contact lens users):
- Keep lenses away from water: remove lenses before showering, swimming, or using a hot tub. Don’t rinse lenses or cases with tap water, bottled water, or saliva. 5
- Use only sterile contact lens solutions: never use non-sterile water or homemade saline. Don’t “top off” old solution in the case; always use fresh solution and replace cases regularly.
- Hand hygiene and schedule: wash and dry hands before handling lenses, follow replacement schedules, and avoid sleeping in lenses unless your eye care provider has specifically approved it. 1
Low-vision resources, tinted lenses, or temporary glasses prescriptions may help with comfort and daily tasks while the eye heals.
Latest Research & Developments
Research is aimed at improving early diagnosis and shortening treatment. Randomized and comparative studies suggest that higher-strength PHMB (0.08%) may be as effective as conventional combination therapy when delivered via standardized protocols, supporting simpler regimens in some settings. 10 Reviews also discuss adjunctive options (such as miltefosine in select refractory cases), the growing role of in vivo confocal microscopy and PCR for diagnosis, and optimization of treatment protocols to target resistant cyst forms. 11
Public-health messages continue to emphasize water-avoidance behaviors for contact lens wearers and fast referral to specialists when AK is suspected.
Recent Peer-Reviewed Research
Diagnostic Accuracy of Clinic-Based Loop-Mediated Isothermal Amplification and Quantitative PCR for Fungal and Acanthamoeba Keratitis.
Cao B, Vu CHV, Le CX, et al.
Polihexanide (PHMB) 0.08% versus currently used treatments for Acanthamoeba keratitis: indirect treatment comparisons.
Papa V, Galeone C, De Francesco M, et al.
Acanthamoeba Keratitis Secondary Glaucoma Associated With Mature Cataract and a Fixed Dilated Pupil in a 40-Eye Series.
Hussain R, Dart JKG, Hamid S
Next Steps
If you have a painful, red eye—especially if you wear contact lenses—seek care promptly. If pain is severe, vision is worsening, or you have light sensitivity, call your eye doctor or go to urgent care/emergency care the same day.
The best specialist to evaluate and treat this condition is a cornea specialist (ophthalmologist). When scheduling, explain that you are a contact lens wearer with a painful red eye and possible Acanthamoeba keratitis. If the clinic is full, ask to be placed on a same-day cancellation list. Some areas require a referral from a primary care provider or optometrist; bringing your contact lens brand, solutions, and case to the visit can help.
You can also connect on Kerbside to be matched to the right specialist for a medical education consult. This is for education and coordination only and does not establish a patient–physician relationship, but it can help you understand tests, treatments, and what to expect.