Trichiasis
Also known as Ingrowing Eyelashes, Misdirected Eyelashes
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
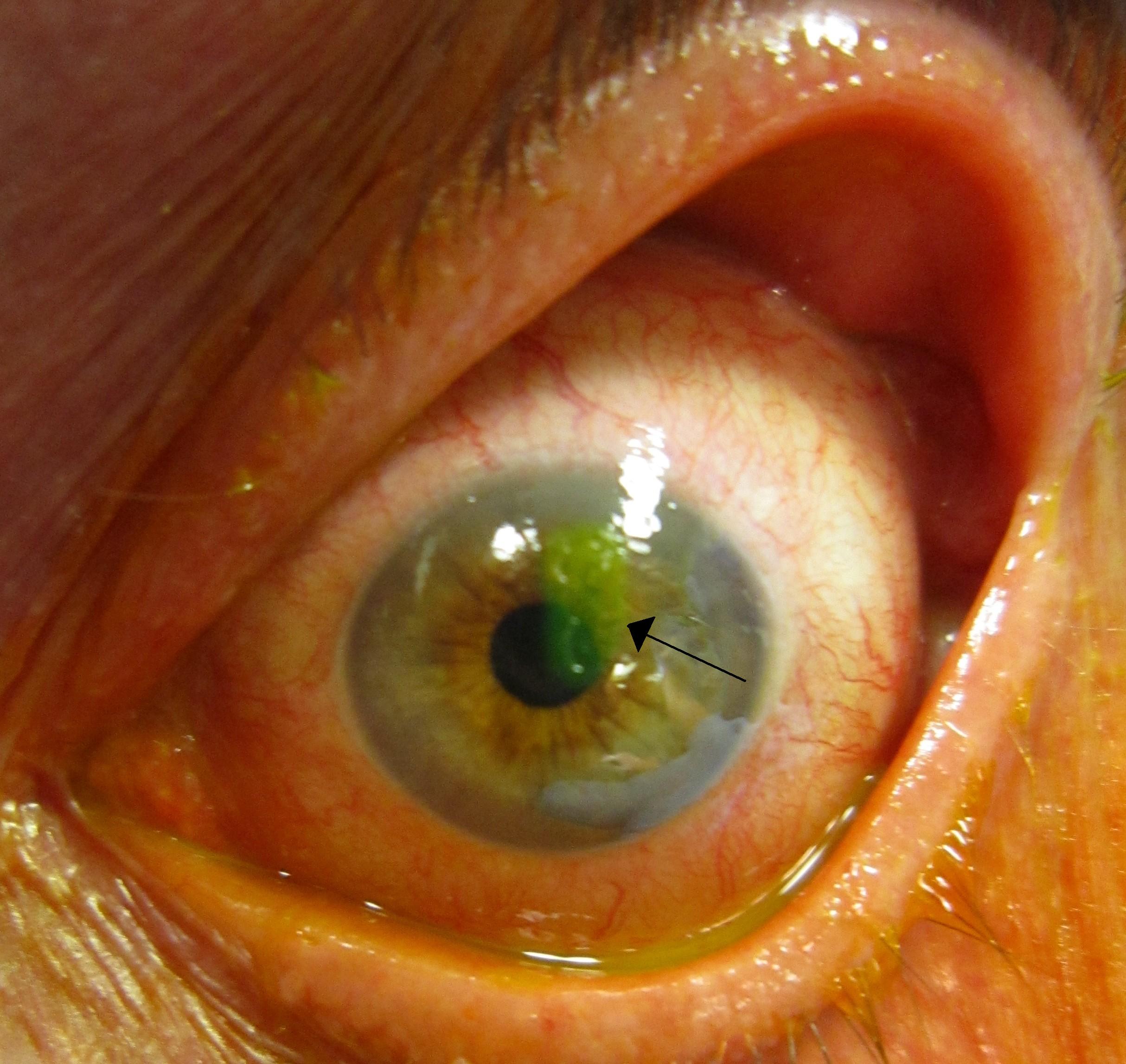
Trichiasis is when one or more eyelashes turn inward and rub against the surface of the eye. This can irritate the eye and, if not treated, may scratch the clear front window of the eye (the cornea). Unlike entropion, where the entire eyelid turns inward, trichiasis involves misdirected lashes with the eyelid position usually remaining normal. Common causes include chronic eyelid inflammation, scarring, and sometimes prior injuries or surgery. In many people, the cause is unknown. Treatments range from simply plucking the misdirected lashes to procedures that permanently destroy the problematic lash roots or surgically reposition the eyelid when needed. 1 2
Symptoms
People with trichiasis often describe a constant sensation that something is in the eye. Other common symptoms include:
- Redness, tearing, and irritation.
- Light sensitivity (photophobia) and blurry vision when the cornea is affected.
- Pain or scratchy feeling that gets worse with blinking.
Because lashes can scrape the cornea, repeated rubbing may lead to abrasions, infections, or scarring that can threaten vision if ignored. Prompt evaluation is important if you notice pain, light sensitivity, or vision changes. 1 2
Causes and Risk Factors
Trichiasis can happen for different reasons:
- Eyelid inflammation such as blepharitis can change lash direction over time.
- Scarring from conditions like Stevens–Johnson syndrome, ocular cicatricial pemphigoid, chemical injuries, or chronic allergies.
- Structural issues such as epiblepharon (a skin fold that pushes lashes inward) or a second row of lashes (distichiasis).
- Trauma or prior eyelid surgery.
- Idiopathic—no clear cause.
In parts of the world where trachoma is common, repeated eyelid infections can scar the inner lid and lead to trichiasis in adulthood. 2 3
Risk of Corneal Injury from Trichiasis (Clinic Triage Tool)
Select your details to estimate risk factors.
Diagnosis
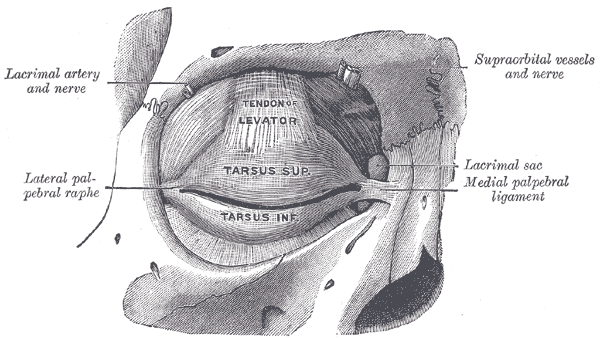
An eye care professional will examine your eyelids and lashes, often using a slit-lamp microscope. They may gently flip the eyelid to check for scarring and look for lashes touching the eye. A special dye called fluorescein can highlight any scratches on the cornea under blue light. It is also important to determine whether the eyelid itself is turning inward (entropion), because that changes the treatment plan. 2
Treatment and Management
Treatment depends on how many lashes are involved, how irritated the eye is, and whether there is underlying scarring or eyelid turning. Options include:
- Lubrication: Artificial tears or ointments can protect the cornea while a plan is made, especially if only one or two lashes are involved. This is a temporary measure.
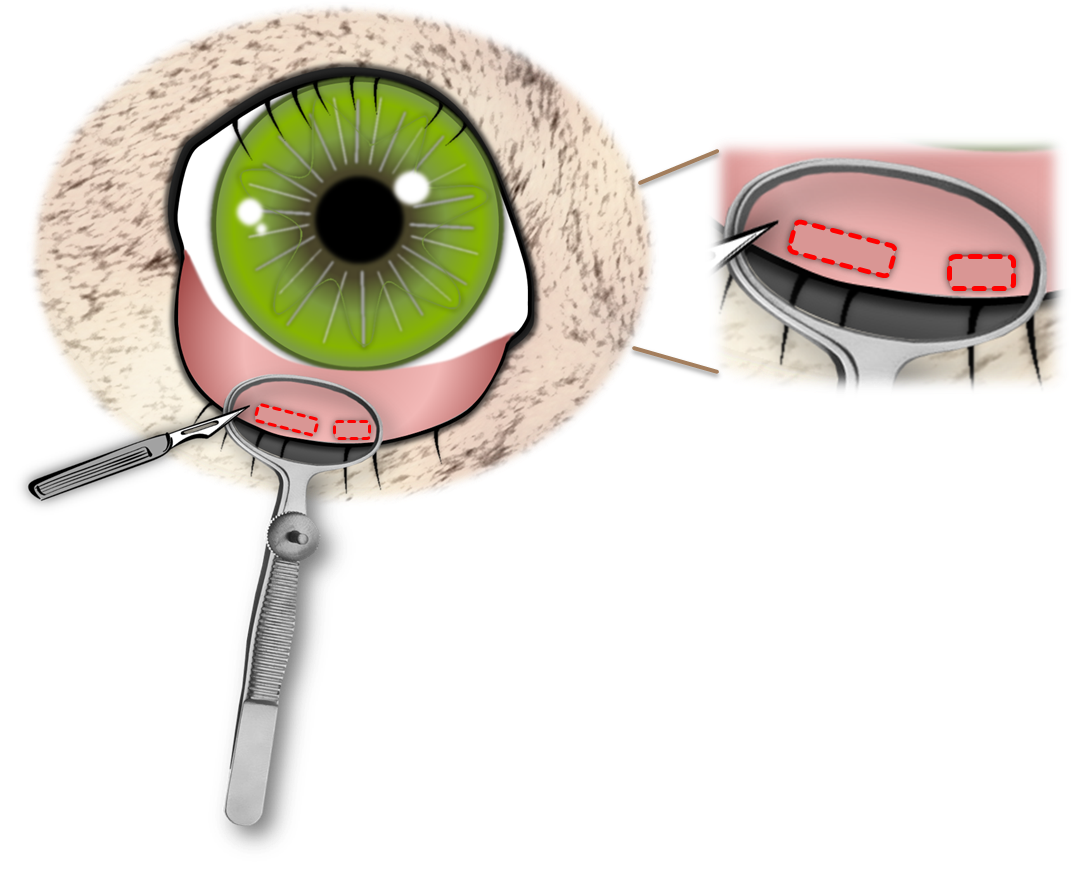
- Epilation (plucking): Quick relief for single or few offending lashes, but they usually grow back in weeks.
- Follicle destruction to prevent regrowth: methods include electrolysis or radiofrequency ablation, laser, or cryotherapy. These aim to permanently stop specific lashes from returning.
- Eyelid surgery: If many lashes are misdirected, if there is scarring, or if the lid is turning in (entropion), a surgical procedure to reposition the lid margin or remove a segment of lash-bearing tissue may be recommended. For trachoma-related trichiasis, large trials suggest some techniques may lower recurrence compared with others.
Your clinician will also treat any underlying causes (for example, managing blepharitis) to reduce the chance of new misdirected lashes. 2
Living with Trichiasis and Prevention
Trichiasis can be frustrating, but most people do well with the right care. Tips:
- Use preservative-free lubricating drops or ointment as advised to protect the cornea while awaiting definitive treatment.
- Avoid plucking lashes yourself—doing this without magnification and proper tools can break the lash, leave stubble that scratches more, or miss other offending lashes. Seek professional care.
- Practice lid hygiene if you have blepharitis (warm compresses and gentle cleansing) as guided by your clinician.
- Wear protective eyewear in dusty or windy environments.
- Seek urgent care if you develop worsening pain, light sensitivity, discharge, or vision changes.
In communities where trachoma is present, public health strategies—often summarized as the SAFE strategy (Surgery, Antibiotics, Facial cleanliness, Environmental improvement)—aim to prevent scarring that can lead to trichiasis. 3 1
Latest Research & Developments
For trachomatous trichiasis, a multicenter trial supported by the U.S. National Eye Institute reported that one eyelid surgery technique (posterior lamellar tarsal rotation, PLTR) reduced recurrence compared with another commonly used technique (bilamellar tarsal rotation, BLTR). This helps programs choose surgical approaches that keep lashes off the eye more reliably.
For non-trachomatous cases with severe scarring, a recent multi-center study compared radiofrequency electro-epilation to eyelash resection and found higher long-term success with eyelash resection in cicatricial ocular surface disease, though multiple interventions may be needed. Your surgeon will tailor the choice to your anatomy and goals. 5
Recent Peer-Reviewed Research
T-Shaped Wedge Resection of the Upper Eyelid: An Alternative to the Pentagonal Wedge.
Ghadiali LK, Zemsky C, Gerber A, et al.
Adnexal surgeries in eyes with keratoprosthesis: challenges and long-term outcomes.
Anklesaria V, Shanbhag SS, Basu S, et al.
Adjunct botulinum toxin for cicatricial pemphigoid.
Mei F, Dallalzadeh LO, Choi P, et al.
Next Steps
If you think you have trichiasis, the best first step is to book an appointment with a comprehensive ophthalmologist (eye MD). If there is scarring or eyelid malposition, you may be referred to an oculoplastic surgeon. When the cornea is scratched or very light sensitive, a cornea specialist may also be involved.
For scheduling: you can self-refer in many areas, but some clinics require a referral from your primary care provider or optometrist. If wait times are long, ask to join a cancellation list, mention if you have pain or vision changes (which may prioritize your visit), and check if a nearby academic center has urgent slots.
You can also connect on Kerbside for a medical education consult with the right specialist to understand your options and likely timelines. This is for education only and does not establish a patient–physician relationship or provide diagnosis or treatment.
Trusted Specialists
Board-certified providers specializing in Trichiasis.
