Preseptal Cellulitis
Also known as Periorbital Cellulitis
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.



Overview
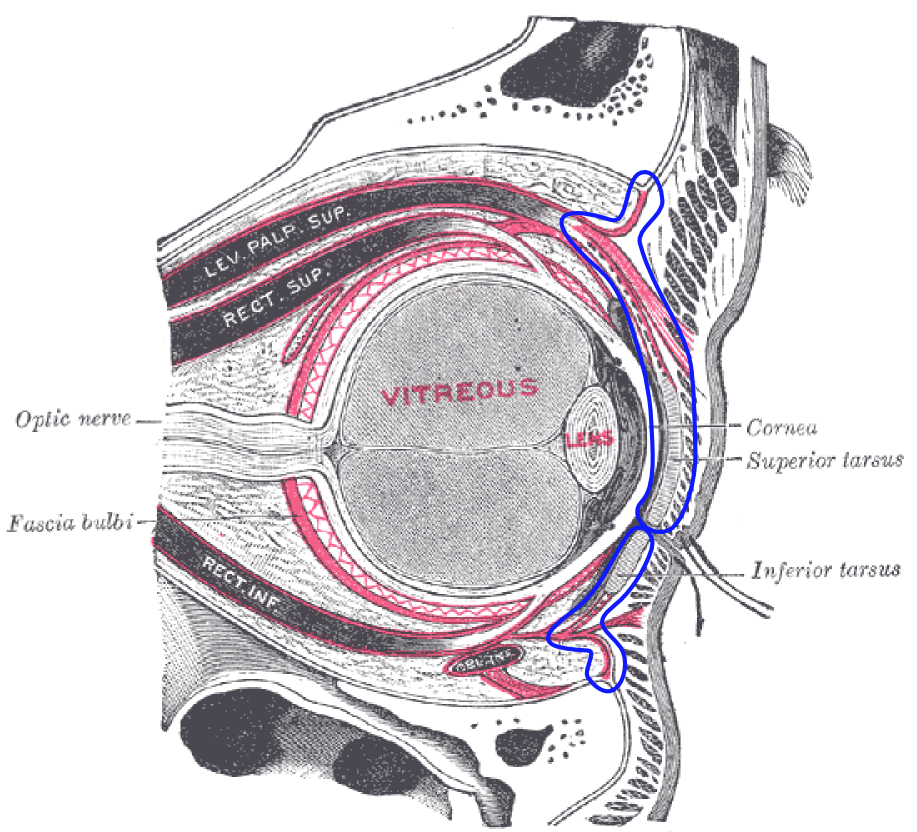
Preseptal cellulitis (also called periorbital cellulitis) is an infection of the eyelid and skin around the eye that stays in front of the orbital septum, a thin barrier that separates the eyelid from the deeper eye socket. It usually causes redness, warmth, and swelling of the eyelids, but it does not affect eye movements or vision when it is limited to the preseptal tissues. With prompt antibiotics, most people recover fully. It is different from orbital cellulitis, a deeper infection behind the septum that can threaten vision and requires urgent hospital care. 1 2
Symptoms
Common symptoms include:
- Eyelid swelling, redness, and tenderness on one side
- Skin that feels warm or tight around the eye
- Sometimes a low-grade fever, especially in children
Go to urgent care or the emergency department now if any of these "red flag" signs are present, because they suggest orbital cellulitis: pain with eye movements, double vision, trouble moving the eye, bulging of the eye (proptosis), reduced vision, or feeling very unwell. 3 4
Causes and Risk Factors
Preseptal cellulitis often starts after bacteria enter through a small break in the skin (like an insect bite or scratch) or spread from a nearby infection such as sinusitis. The most common bacteria are Staphylococcus aureus (including MRSA in some areas), Streptococcus pyogenes, and Streptococcus pneumoniae. 2
Young children are affected more often. In places where the Haemophilus influenzae type b (Hib) vaccine is not widely used, Hib can also cause cases. Keeping children up to date on Hib vaccination reduces the risk of invasive Hib disease, which historically included eye-area infections. 6
Preseptal Cellulitis: Complication / Escalation Risk (assumptive model)
Select your details to estimate risk factors.
Diagnosis
Clinicians diagnose preseptal cellulitis by listening to your symptoms and examining the eyelids and eyes. Most cases do not need blood tests or scans. If any red flags for orbital cellulitis are present, or if the swelling is severe or not improving, a CT or MRI may be ordered to check for deeper infection or complications. Children who are very young or appear unwell are assessed more cautiously and may need hospital observation. 3 1
Treatment and Management
Treatment depends on age, severity, and local antibiotic resistance patterns. Many people with mild illness can be treated at home with oral antibiotics that cover common skin and sinus bacteria (for example, amoxicillin–clavulanate). If there is a risk of community MRSA, clinicians may choose clindamycin or trimethoprim–sulfamethoxazole combined with a beta-lactam to ensure adequate Streptococcus coverage. Typical duration is 5–7 days, extended if symptoms persist. Close follow-up within 24–48 hours is important to make sure swelling and redness are improving. 7
Hospital care with IV antibiotics is recommended for infants (especially under 1 year), people who look systemically unwell, those who cannot take oral medicines, and anyone with possible orbital involvement. Eye doctors (ophthalmologists) and sometimes ENT or infectious disease specialists may be involved. Imaging and surgery are considered if an abscess or sinus complication is suspected. 3
Living with Preseptal Cellulitis and Prevention
Most people feel better within a day or two of starting the right antibiotic. Keep the area clean, avoid rubbing the eyelids, and use warm compresses if they feel soothing. Take medicines exactly as prescribed and finish the full course.
- When to recheck: call your clinician if symptoms are not clearly improving in 24–48 hours, if new fever develops, or if any red flags (eye pain with movement, double vision, vision changes, or bulging) appear. 4
- Lower your risk: promptly clean and cover cuts around the eye, treat sinus symptoms early, and keep routine childhood immunizations—especially Hib—up to date. 6
Latest Research & Developments
Today, fewer cases in young children are linked to Hib because of widespread vaccination. Current literature also emphasizes careful screening for MRSA where it is prevalent and rapid escalation to imaging and IV therapy when orbital signs are present. 2 Pediatric centers increasingly use standardized care pathways that spell out when to image, which antibiotics to choose, and how quickly to step down to oral therapy—an approach shown to streamline care and support good outcomes. 8
Recent Peer-Reviewed Research
Frontal osteomyelitis presenting as chronic preseptal abscess: an unusual scenario.
Hosny R, Younan A, Ahmed RA
Effect of Prophylactic Topical Antibiotics on Rates of Infectious Complications After Strabismus Surgery: A Large Database Study.
Binczyk NM, Koo EB, Lambert SR
The profile of patients attending to the general emergency department with ocular complaints within the last year: is it a true ocular emergency?
Dag Y, Aydın S, Kumantas E
Next Steps
If you think you or your child has preseptal cellulitis, seek medical care promptly. The best specialist to evaluate and manage this condition is a ophthalmologist (ideally pediatric ophthalmology or oculoplastic-trained), working closely with your primary care clinician. In some cases, an ENT or infectious disease specialist may be involved.
How to schedule: start with your primary care doctor or urgent care for same-day assessment. They can start treatment and, if needed, place a referral to ophthalmology. If appointment times are limited, ask about waitlists and same-day cancellation slots. Go to the emergency department immediately if there are any red flags (eye pain with movement, double vision, vision loss, or bulging), if the patient is an infant, or if symptoms are rapidly worsening.
Need help finding the right expert? You can connect directly with the appropriate specialist on Kerbside for a medical education consult about your case (this is educational support and does not create a patient–physician relationship).