Herpes Simplex Keratitis
Also known as Ocular Herpes
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
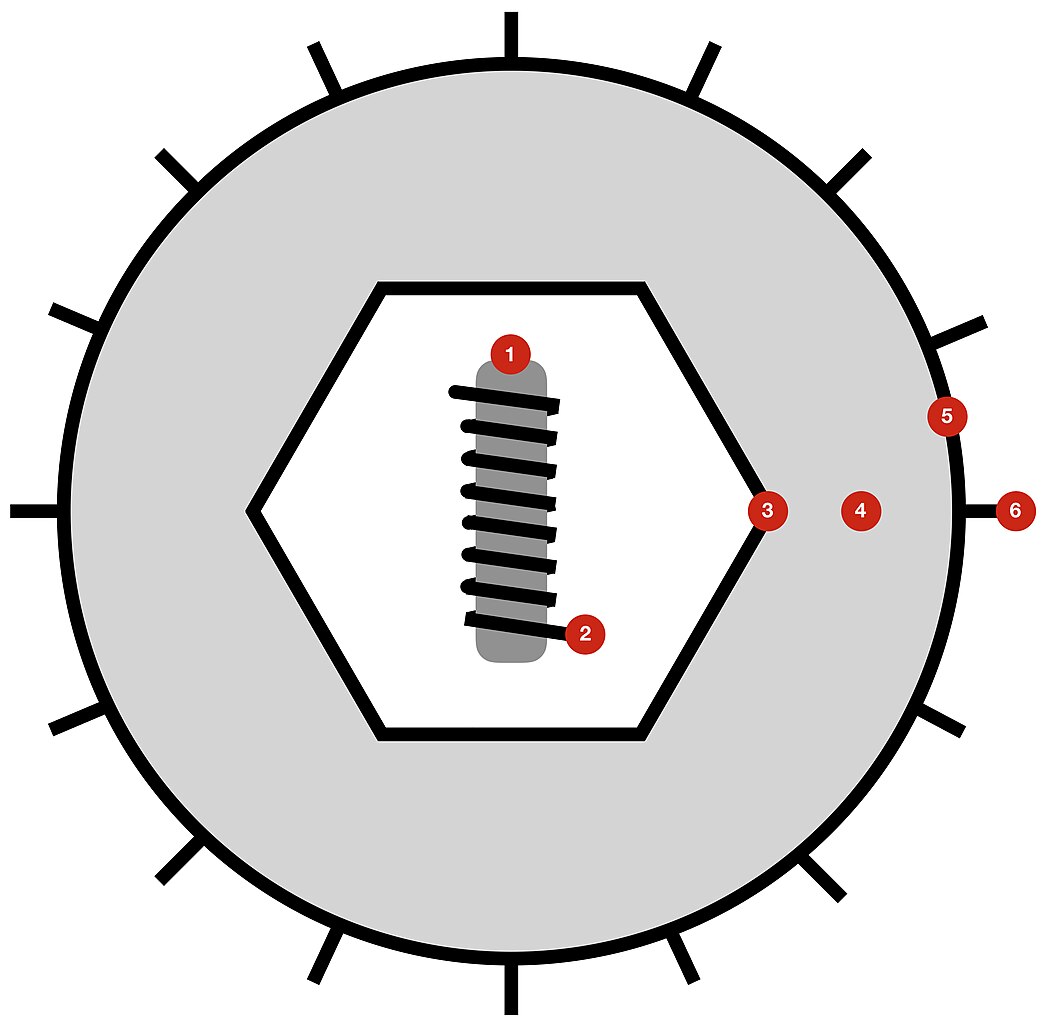
Herpes simplex keratitis (HSK) is an infection of the cornea—the clear front window of the eye—most often caused by herpes simplex virus type 1 (HSV-1). 1
After an initial infection, the virus can go quiet (dormant) in a nearby nerve and later flare again, which is why some people have repeat episodes over time. 1
Flares can be mild and just affect the surface, or they can inflame deeper layers and leave scars that blur vision. With prompt diagnosis and the right treatment plan, most people heal well and protect their sight; learning your triggers and acting early makes a big difference. 2
Symptoms
HSK usually affects one eye at a time. Symptoms can start suddenly or build over a day or two. 3
Common signs:
- Sore or gritty feeling
- Redness and tearing
- Light sensitivity
- Blurry vision
- Halos around lights
- Sensation like an eyelash is stuck
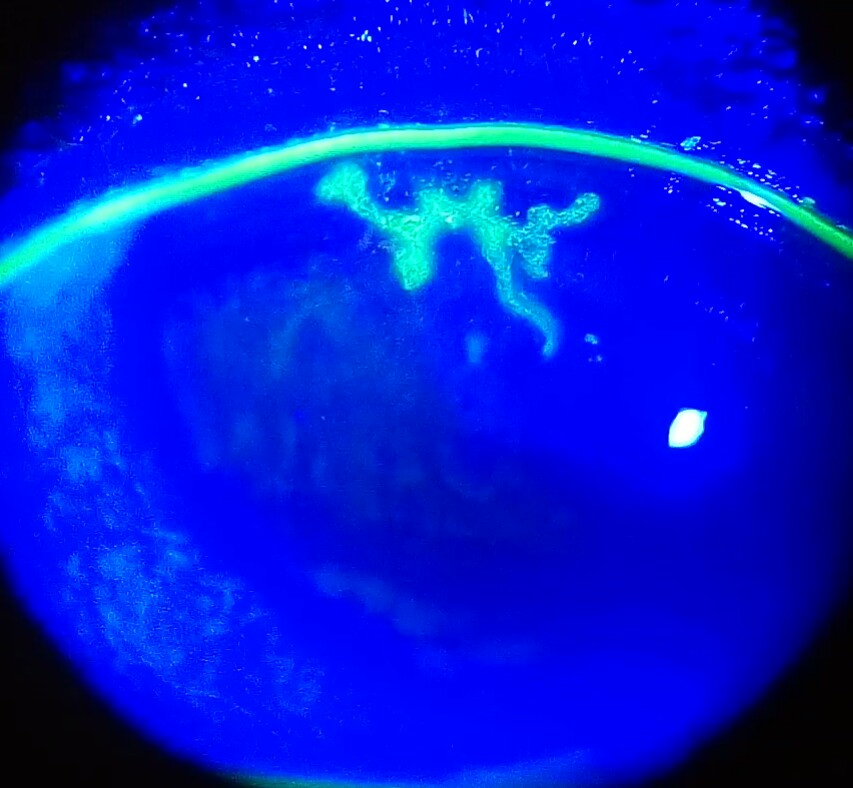
During the exam, eye doctors often see a classic branching sore (a dendrite) on the corneal surface that takes up fluorescein dye. 1
Call the same day if you have severe pain, sudden vision changes, or a very red, light-sensitive eye, and pause contact lenses until an eye doctor says it is safe. 3
Causes and Risk Factors
Most eye herpes comes from HSV-1, the same virus that causes cold sores around the mouth. 2 After a past exposure, the virus can reactivate and travel along the nerve to the cornea.
Common triggers:
- Fever or illness
- Stress
- Intense sunlight/UV
- Eye surgery or injury
- Weakened immune system
Key safety point: Steroid eye drops without antiviral coverage can make surface (epithelial) HSK worse and should only be used when an eye specialist says so. 1
HSK Flare Risk (Educational)
Select your details to estimate risk factors.
Diagnosis
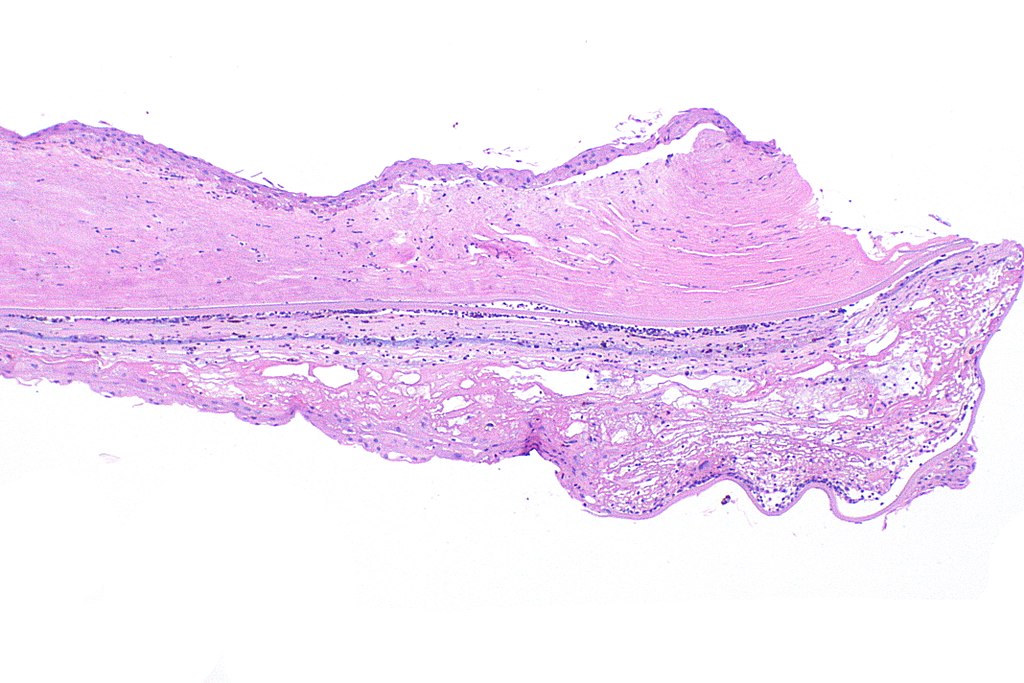
Eye doctors diagnose HSK with a slit-lamp microscope exam. They may place fluorescein dye to highlight a dendritic ulcer on the surface, check corneal sensation (often reduced in HSK), and look for deeper signs such as stromal haze, tiny deposits on the back of the cornea, or inflammation inside the eye.
When the picture is unclear—or another infection is possible—a gentle swab may be sent for PCR to confirm the virus. Early, accurate diagnosis guides safe therapy and helps prevent scarring. 1
Treatment and Management
Treatment depends on which corneal layer is involved and how severe the flare is.
- Epithelial HSK (surface infection): Antiviral gel or drops (e.g., ganciclovir, trifluridine) and often an oral antiviral (acyclovir or valacyclovir). Steroid eye drops are avoided in active epithelial disease because they can worsen it. 1
- Stromal or endothelial HSK (deeper inflammation): Immune-driven; typical care combines a topical steroid to calm inflammation plus an antiviral (topical or oral) to suppress virus. Taper doses slowly to prevent rebound. 1
- Prevention of recurrences: For frequent flares—especially after stromal disease—daily oral acyclovir for a year can help. The NIH-funded HEDS study found suppressive acyclovir reduced new episodes and protected vision. 4
Living with Herpes Simplex Keratitis and Prevention
A few practical steps can lower your chance of another flare and help you heal faster if one starts:
- Act quickly: If you notice pain, light sensitivity, or a sudden blur, stop contact lenses and call your eye doctor the same day.
- Protect your eyes: Wear sunglasses outdoors to reduce UV and wind exposure; use preservative-free artificial tears if your eyes feel dry.
- Use medicines exactly as prescribed: Never restart leftover steroid drops on your own; ask your doctor before using new eye drops.
- Practice contact lens hygiene: Replace lenses and cases as directed, avoid sleeping in lenses unless approved, and avoid water exposure while wearing them. 5
Most people who follow a plan, keep follow-ups, and manage triggers maintain excellent vision over time; learn the warning signs of keratitis and seek care early if symptoms return. 6
Latest Research & Developments
Scientists are exploring ways to prevent flares and protect the cornea beyond standard antivirals.
Recent Peer-Reviewed Research
Tear metabolomics reveals novel potential biomarkers in epithelial herpes simplex keratitis.
Zhang J, Wu Z, Zhang Y, et al.
Exploring Heparanase Levels in Tears: Insights From Herpes Simplex Virus-1 Keratitis Patients and Animal Studies.
Gagan S, Khapuinamai A, Kapoor D, et al.
Loss of TRPM8 Exacerbate Herpes Simplex Keratitis Infection in Mice by Promoting the Infiltration of CD11b+ Ly6G+ Cells and Increasing the Viral Load in the Cornea.
Feng J, Yang L, Ran L, et al.
Next Steps
If you have new redness, light sensitivity, or blurry vision—especially if you have had HSK before—seek a same-day exam with an ophthalmologist (ideally a Cornea specialist). Tell the scheduler you have possible herpes simplex keratitis so they can try to fit you in urgently. 3
If the first clinic is full, ask about cancellation lists or an on-call doctor, and keep all follow-ups so your clinician can confirm healing and safely taper drops. Most patients with HSK are managed by an ophthalmologist, and some will need longer-term prevention to cut the risk of flares. 1
You can also connect on Kerbside for a medical education consult with the right specialist (no patient–physician relationship is established).
Trusted Specialists
Board-certified providers specializing in Herpes Simplex Keratitis.
