Pinguecula
Also known as Surfer’s Bump
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.


Overview
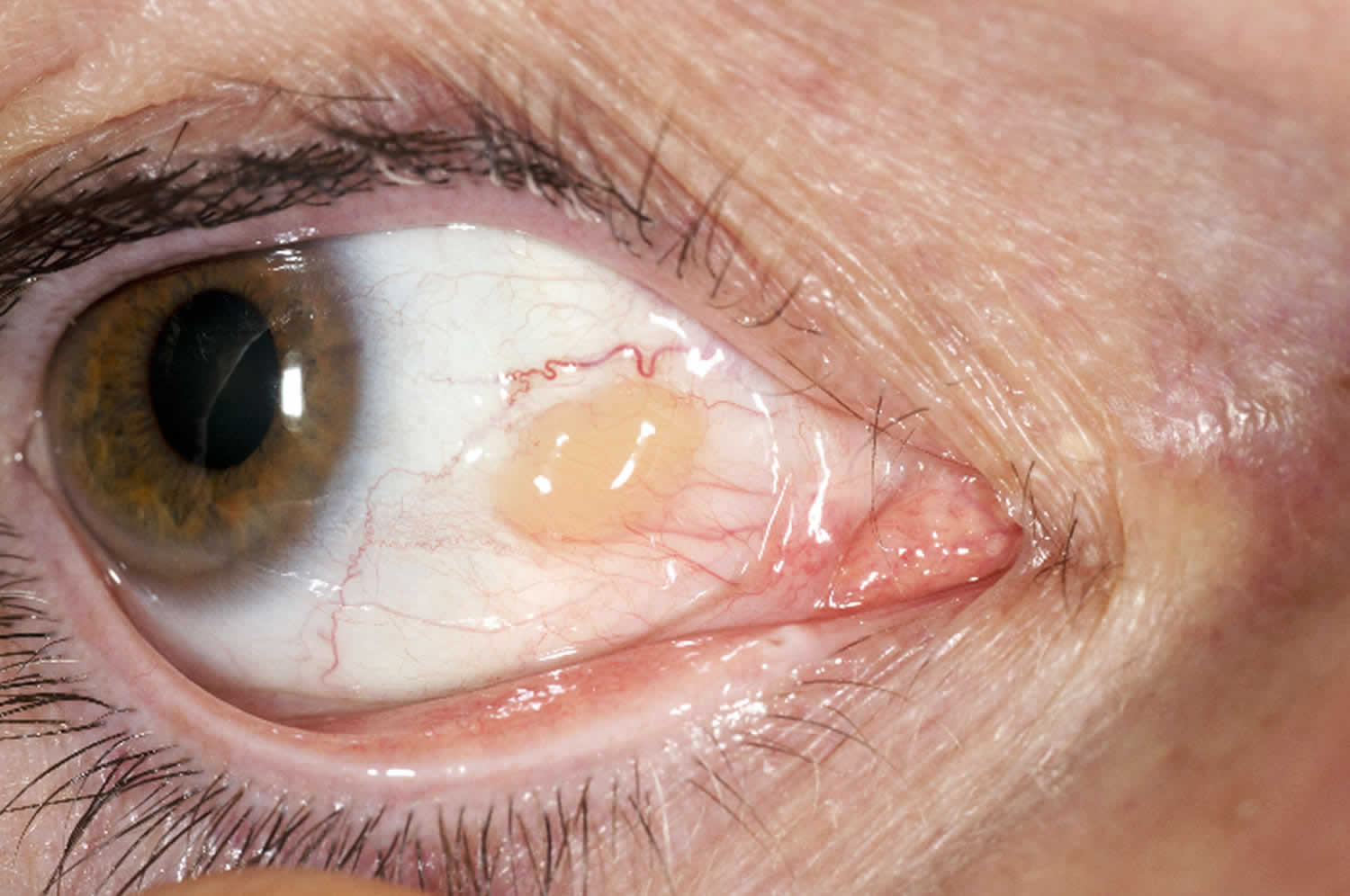
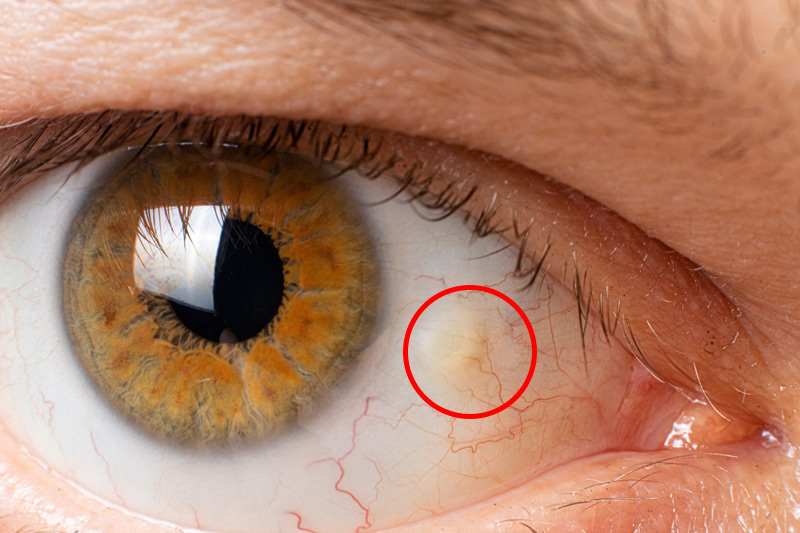
Pinguecula (pronounced ping-GWEH-kyuh-luh) is a small, yellow-white, slightly raised patch that forms on the clear membrane (conjunctiva) covering the white of your eye, usually on the side closest to your nose. The bump represents sun- and wind-related degeneration of collagen and elastin fibers inside the tissue. Although it can look alarming, a pinguecula is benign and rarely threatens vision.1 The spot may stay tiny for life, or very slowly enlarge; in a small percentage of people it can give rise to a larger, triangular growth called a pterygium.2 Early recognition matters because simple protections—UV-blocking sunglasses, lubricating drops, and avoidance of dusty, dry environments—can keep the lesion quiet and comfortable.
Symptoms
Most pingueculae produce no symptoms and are discovered during a routine eye exam. When people do notice something, it is usually one or more of the following:
- Visible yellow spot or bump on the white of the eye, often nearest the nose.3
- Dryness, burning or a gritty sensation—the elevation can disrupt the normal tear film.1
- Redness and swelling when the tissue becomes inflamed, a flare-up called pingueculitis.
- Foreign-body feeling or contact-lens intolerance if the lens edge rubs the bump.4
Pain, loss of vision, or rapid growth are not typical; their presence should prompt urgent specialist review to rule out infection or other ocular surface tumors.
Causes and Risk Factors
Researchers believe pingueculae form when chronic environmental stress alters conjunctival collagen. Key contributors include:
- Ultraviolet (UV) light exposure—outdoor work and recreation near sand, water or snow amplify reflected UV rays.5
- Dry, windy, dusty climates that mechanically irritate the ocular surface.1
- Increasing age—degenerative changes accumulate over decades.2
- Unprotected contact-lens wear and chronic eye-rub or allergy.
- Outdoor occupations (farmers, fishers, lifeguards) or high-altitude living.
- Co-existing dry-eye disease that leaves the conjunctiva less lubricated and more prone to micro-injury.6
Pinguecula Risk Score
Select your details to estimate risk factors.
Diagnosis
An eye-care professional can diagnose a pinguecula in minutes:
- Slit-lamp examination reveals a slightly elevated, yellow-white mound that stops at the corneal edge, distinguishing it from a pterygium.3
- Fluorescein dye may highlight tear-film disruption and help assess dryness.
- Photography or anterior-segment OCT (optional) documents size for future comparison.
- Biopsy or referral is reserved for unusual pigmentation, rapid growth, or suspicion of conjunctival neoplasia.9
Routine eye exams—starting at school age and repeating every 1-2 years—are the best way to detect asymptomatic lesions early.
Treatment and Management
Because most pingueculae are harmless, treatment focuses on comfort and prevention:
- Lubricating artificial tears 3-4 times daily ease dryness and foreign-body sensation.1
- Sunglasses with 99-100 % UVA/UVB blocking wraparound lenses reduce further UV damage.5
- Topical anti-inflammatory drops (short-course corticosteroid or ciclosporin) calm pingueculitis flares.8
- Soft-bandage contact lenses can shield the bump in severe irritation.
- Surgical excision—performed by a cornea specialist under local anesthesia—is reserved for persistent inflammation, cosmetic concerns, or if the lesion threatens to encroach on the cornea.7
Recurrence after removal is uncommon but possible; meticulous UV protection lowers that risk.
Living with Pinguecula and Prevention
Day-to-day strategies can keep eyes comfortable and reduce the chance of the bump growing:
- Follow the 20-20-20 rule—every 20 minutes at a screen, look 20 feet away for 20 seconds—to stimulate blinking.
- Apply preservative-free lubricating drops during windy, dusty, or low-humidity days.4
- Wear broad-brimmed hats and quality sunglasses whenever the UV index is moderate or higher.5
- Use protective goggles for yard work, sanding, or water sports.
- Quit smoking and moderate alcohol; both can worsen ocular-surface dryness.
- Schedule annual eye exams if you are an outdoor worker or have a history of dry eye.
With these measures, most people never need surgery and may even forget the spot is there.
Latest Research & Developments
Scientists are exploring new ways to prevent and treat UV-related conjunctival disease:
- UV-spectrum absorbing contact-lens materials under development could shield the limbal conjunctiva more effectively than today’s lenses.7
- Anti-inflammatory nanodrop formulations aim to deliver corticosteroids only to inflamed tissue, minimizing side-effects.
- Gene-expression profiling has identified up-regulation of matrix metalloproteinases during pingueculitis, opening doors for targeted biologic therapies.6
- Smart-phone UV-exposure apps linked to wearable light sensors are being tested to reinforce sun-safety behaviors in surfers and lifeguards.
- Clinical trials supported by the National Eye Institute are evaluating whether low-dose topical ciclosporin can prevent progression from pinguecula to pterygium in high-risk populations.5
Recent Peer-Reviewed Research
Detection of Ocular Surface Squamous Neoplasia Using Artificial Intelligence With Anterior Segment Optical Coherence Tomography.
Greenfield JA, Scherer R, Alba D, et al.
Anterior Segment Swept-Source Optical Coherence Tomography in Ocular Surface Tumors and Simulating Lesions and Correlation With Histopathologic Diagnosis.
Gündüz AK, Mirzayev I, Ersöz CC, et al.
Ocular Surface Squamous Neoplasia Masquerading as Recalcitrant Epithelial Keratitis.
Watane A, Hansen ED, Vazquez LE, et al.
Next Steps
If the bump becomes red, grows toward the cornea, or interferes with contact-lens wear, the ideal provider is a cornea and external-disease specialist. These ophthalmologists have advanced microsurgical training and access to amniotic-membrane grafts, tissue-sparing lasers, and customized anti-inflammatory protocols.
How to schedule: You can ask your optometrist or primary eye doctor for a referral, but many tertiary eye centers allow self-referral. Appointment availability may vary, so consider virtual triage or second opinions through Kerbside to connect quickly with board-certified subspecialists and learn whether observation, drops, or removal is best for you.
Trusted Specialists
Board-certified providers specializing in Pinguecula.
