Nystagmus
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
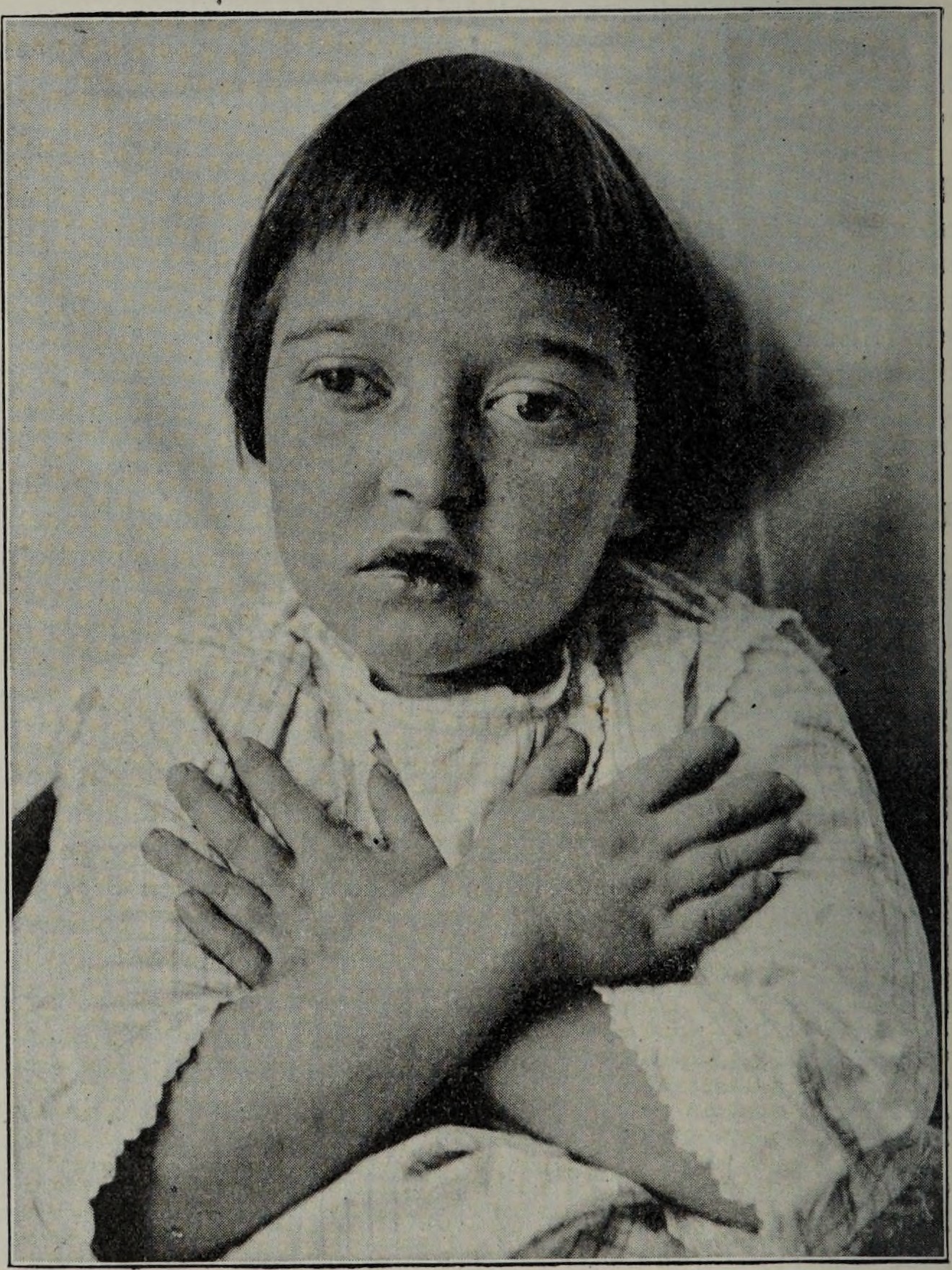
Nystagmus is an involuntary, repetitive movement of one or both eyes that can be horizontal, vertical, rotary, or mixed in direction. These motions interfere with the eye’s ability to hold steady fixation, so images may appear to oscillate or blur. Nystagmus can be congenital—noticed in the first few months of life—or acquired later due to ocular, vestibular, or neurologic disease. Although estimates vary, population studies suggest roughly 6–24 people per 10,000 are affected.1 In many infants, nystagmus is isolated and non-progressive, but adults who suddenly develop the condition should be evaluated promptly, since it can signal serious underlying problems.2
Symptoms
- Rhythmic, uncontrollable eye movements (jerk or pendular)
- Shaky or blurred vision, especially when trying to focus on a target
- Oscillopsia—the sensation that the surrounding world is moving
- Poor depth perception and difficulty with balance or coordination
- Head turn or tilt to a “null point” where movements are dampened
- Light sensitivity, night-vision problems, or dizziness in acquired forms
Symptom severity can fluctuate with fatigue, stress, or gaze position, and many people with congenital nystagmus are unaware of the motion until it is pointed out.1 Acquired nystagmus, by contrast, often produces disabling oscillopsia and vertigo.2
Causes and Risk Factors
Common causes
- Genetic mutations—FRMD7 is strongly linked to X-linked infantile nystagmus.3
- Albinism, optic nerve or retinal disorders, cataract, or severe refractive error
- Inner-ear disease (e.g., benign paroxysmal positional vertigo, Ménière’s)
- Neurologic conditions such as multiple sclerosis, stroke, tumors, trauma
- Medications or toxins: antiseizure drugs, alcohol, sedatives
Risk is higher in premature infants, children with visual-development disorders, and anyone with vestibular or neurologic disease. In adults, a sudden onset demands urgent evaluation to rule out stroke or demyelination.12
Nystagmus Functional Impact Score
Select your details to estimate risk factors.
Diagnosis
A comprehensive eye and neurologic exam comes first. Key tools include:
- Electronystagmography (ENG) — surface electrodes record eye-muscle potentials to quantify direction, frequency, and velocity.4
- Videonystagmography (VNG) — infrared goggles capture eye movements in the dark and during positional maneuvers.5
- Optical coherence tomography, visual-evoked potentials, or ERG to assess retinal or optic-nerve integrity
- MRI or CT of brain and orbit when central causes are suspected
- Targeted genetic testing in familial or infantile cases
These studies help classify nystagmus (jerk vs. pendular, gaze-evoked, vestibular, etc.) and guide therapy.
Treatment and Management
No single cure exists, but many patients achieve meaningful improvement.
- Correct underlying problems (e.g., treat inner-ear disease, control MS relapse).
- Optical approaches: glasses, contact lenses, or prism lenses to sharpen vision and minimize null-point head turns.1
- Medications: gabapentin, baclofen, memantine, or botulinum toxin may dampen oscillations in acquired forms.
- Eye-muscle surgery: recess-resect or four-muscle procedures can shift the null zone and reduce head posture.
- Low-vision rehabilitation: magnifiers, large-print materials, and orientation-mobility training.
Therapy is highly individualized; combining optical, pharmacologic, and surgical strategies often yields the best functional outcome.2
Living with Nystagmus and Prevention
Daily strategies
- Use good lighting and high-contrast text to ease reading.
- Position reading material at the null point; some people benefit from a stand or adjustable monitor.
- Take regular visual breaks to reduce fatigue-induced oscillations.
- Practice balance exercises or vestibular therapy if dizziness is problematic.
- Wear protective eyewear during sports to prevent trauma-triggered worsening.
Because congenital nystagmus is largely non-preventable, early detection and prompt referral to eye care and low-vision services are critical for maximizing visual development.12
Latest Research & Developments
Research is rapidly expanding in three key areas:
- Gene-targeted therapy. Several labs are exploring viral vectors to deliver healthy FRMD7 copies in X-linked infantile nystagmus, building on proven retinal-gene-therapy platforms.3
- Sensor-based home training. Wearable eye trackers and virtual-reality headsets are being studied to provide personalized ocular-motor exercises that may enhance visual stability.
- Artificial-intelligence diagnostics. NEI-funded teams are leveraging deep-learning algorithms to quantify nystagmus waveforms and monitor drug response more precisely.6
Clinical-trial enrollment is ongoing; ask your ophthalmologist about emerging studies.
Recent Peer-Reviewed Research
Disrupted Motor Neuron and Neuromuscular Junction Development in an Albino Mice Model of Infantile Nystagmus.
Vemula S, Osman A, Yang X, et al.
Expansion of the ABCA4-Associated Retinopathy Spectrum: Severe Variants Can be Associated With Early-Onset Severe Retinal Dystrophy.
Panneman DM, Hitti-Malin RJ, McKibbin M, et al.
Clinical manifestations of dual-gene variants involving ABCA4 in retinal dystrophies.
Wolfram L, Merle DA, Kühlewein L, et al.
Next Steps
If you notice new eye shaking, blurred vision, or balance changes, schedule an appointment with a neuro-ophthalmologist—a specialist trained in eye–brain disorders. Your primary-care physician or optometrist can provide a referral, but self-referral is often possible at major centers such as Mayo Clinic’s neuro-ophthalmology service.7 Expect a detailed history, dilated eye exam, and possibly imaging or electrophysiology on your first visit. Wait times vary; calling multiple regional centers or using online portals may speed access. You can also connect with the right specialist on Kerbside for an educational consult (no patient-physician relationship will be established), which can help you gather records and clarify questions before a formal visit.