Idiopathic Intracranial Hypertension
Also known as IIH
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
Idiopathic intracranial hypertension (IIH) happens when the pressure of the fluid around your brain (cerebrospinal fluid, or CSF) is too high without a clear cause. People often have daily headaches, vision changes (like brief dimming or double vision), and swelling of the optic nerves in the back of the eyes (papilledema). IIH is most common in women of childbearing age with overweight or obesity, but anyone can develop it. Early diagnosis and treatment help protect vision and improve quality of life. 1 2
Symptoms
Common symptoms include:
- Headache (often daily, worse when lying down or first thing in the morning).
- Visual changes such as brief vision dimming (transient visual obscurations), blurred vision, double vision, or loss of side vision. Light flashes and whooshing sounds in the ears (pulsatile tinnitus) are also reported.
- Nausea/vomiting with severe pressure spikes.
On exam, clinicians often see papilledema, which is swelling of the optic disc caused by high intracranial pressure and a major warning sign for vision risk. Prompt evaluation is important to protect sight and rule out other causes of increased pressure. 3 4
Causes and Risk Factors
In IIH, the brain and spinal fluid pathways look normal on imaging, but CSF pressure is elevated. The exact cause is unknown (that’s what “idiopathic” means). Well-recognized risk factors include having overweight or obesity, recent weight gain, being female of childbearing age, and conditions like obstructive sleep apnea. Certain medicines can raise risk for intracranial pressure problems and IIH-like syndromes, including tetracycline-class antibiotics and vitamin A derivatives (for acne), as well as growth hormone. 6
IIH Risk (Educational)
Select your details to estimate risk factors.
Diagnosis
Doctors use a step-by-step approach:
- Eye exam: looks for papilledema and checks visual acuity and visual fields.
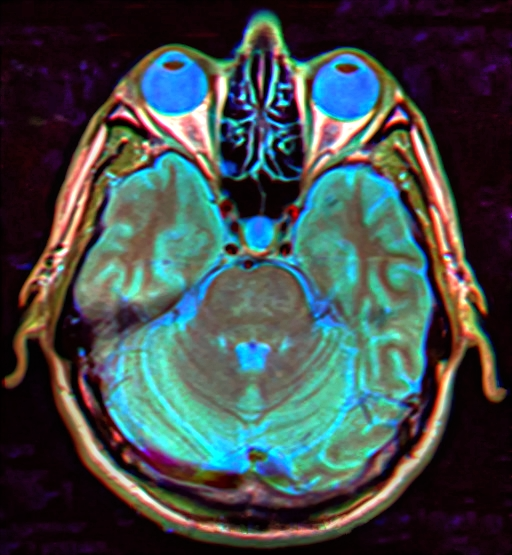
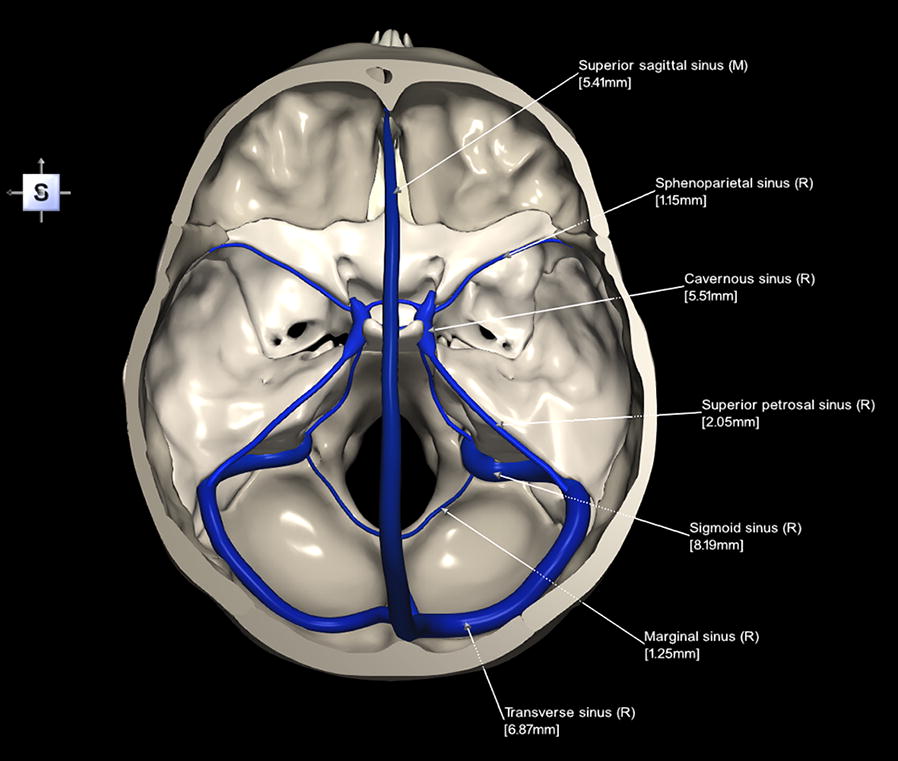
- Brain MRI (often with MRV): rules out mass, hydrocephalus, and venous sinus thrombosis; may show signs linked with IIH (e.g., empty sella, optic nerve sheath enlargement).
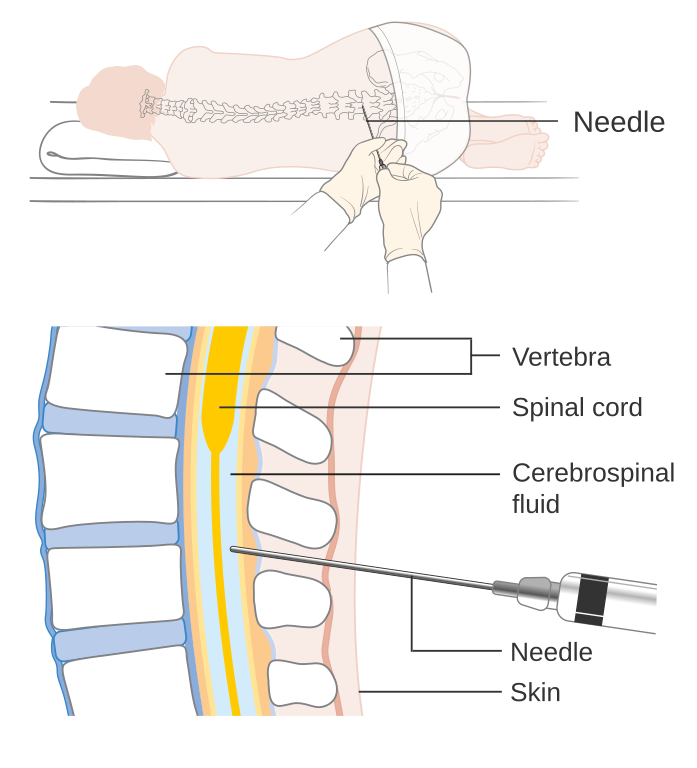
- Lumbar puncture: measures CSF opening pressure (elevated in IIH) and confirms normal CSF contents.
Imaging first is important, then lumbar puncture confirms the diagnosis and guides treatment planning. 7 8
Treatment and Management
The goals are to protect vision and reduce symptoms. Your plan is personalized and may include:
- Weight reduction: Even a 5–10% weight loss can help lower pressure and symptoms. For some with severe obesity, bariatric surgery may be considered.
- Medicines: The first-line drug is often acetazolamide (a carbonic anhydrase inhibitor) to reduce CSF production. Topiramate can be helpful for headaches and may aid weight loss.
- Lumbar puncture: Occasionally used therapeutically to temporarily lower pressure.
- Procedures: If vision worsens or pressure stays high despite medical therapy, options include optic nerve sheath fenestration (to protect vision) or CSF shunting. In selected cases with venous sinus stenosis and a significant pressure gradient, venous sinus stenting may be considered by a multidisciplinary team.
Most people improve with medication and weight management; procedures are reserved for vision-threatening or refractory cases. 9 10
Living with Idiopathic Intracranial Hypertension and Prevention
You can take practical steps to lower pressure swings and protect your sight:
- Know your warning signs: sudden vision dimming, new double vision, or a dark curtain in part of your vision needs same-day care.
- Build a headache plan: track triggers (sleep, hydration, stress), and review safe pain strategies with your clinician.
- Weight, sleep, and meds: gradual weight loss, treating sleep apnea, and avoiding pressure-raising medicines (like tetracyclines or vitamin A derivatives) when possible can help.
- Keep follow-ups: visual field testing tracks small changes you may not notice day to day.
Partner with your eye and neurology teams to adjust treatment as life changes. Many people return to regular activities with the right plan and monitoring. 11 12
Latest Research & Developments
New evidence helps refine care. A major 2018 consensus guideline outlines best practices across diagnosis, vision protection, and when to consider procedures such as venous sinus stenting. It emphasizes weight loss, acetazolamide as first-line therapy, and close vision monitoring. 13 A randomized clinical trial in JAMA Neurology found bariatric surgery produced greater and sustained reductions in intracranial pressure and weight compared with a community weight program in women with IIH and high BMI, supporting aggressive weight-loss strategies in appropriate candidates. 14
Recent Peer-Reviewed Research
Trends in Prenatal Exposure to Antiseizure Medications Over the Past Decade: A Nationwide Study.
Shahriari P, Drouin J, Miranda S, et al.
Visual field defects in children with brain tumors.
Boethun A, Nordhjem BJT, Mathiasen R, et al.
Anti-dipeptidyl-peptidase-like protein-6 antibody-associated encephalitis masquerading as weight loss and confusion: a case report.
Sefcsik V, Rodriguez P, Makar M, et al.
Next Steps
If you have symptoms suggestive of IIH, seek care promptly. The best specialist to see is a neuro-ophthalmologist (or an ophthalmologist with neuro-ophthalmology expertise) working closely with a neurologist. Start by calling your eye doctor or primary care clinician; ask for an urgent appointment if you notice new vision changes. Imaging is usually performed before a lumbar puncture. You can also connect with the right specialist on Kerbside for a medical education consult (no patient–physician relationship will be established). For red-flag symptoms like sudden vision loss, severe headache with vomiting, or rapidly worsening double vision, get same-day care. 15 16