Fuchs’ Corneal Dystrophy
Also known as FECD
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.

Overview
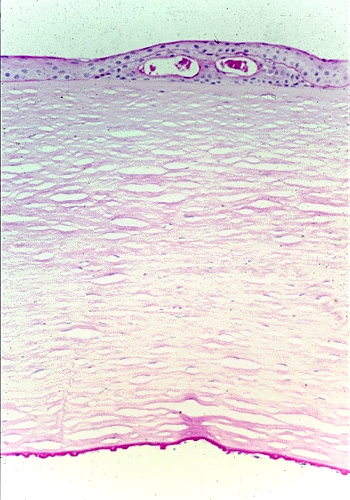
Fuchs’ corneal dystrophy (FECD) is a slow-progressing disease in which the innermost layer of the cornea (the endothelium) gradually loses cells. These cells normally pump fluid out of the cornea to keep it clear. As pumps fail, fluid builds up, the cornea swells, and vision looks hazy—much like a foggy bathroom mirror.1 FECD affects about 4 % of adults over 40 and is the top reason for corneal transplantation in the United States.2 Women are affected twice as often as men, and the condition often runs in families due to variants in the TCF4 or COL8A2 genes.3
Symptoms
- Blurry or cloudy vision on waking that clears through the morning as fluid evaporates
- Glare and halos around lights, especially at night
- Reduced contrast and color saturation
- Eye discomfort or foreign-body sensation when tiny fluid-filled blisters (bullae) form on the corneal surface
- Gradual decline in best-corrected visual acuity
Symptoms usually appear in the 50s or 60s, but early “guttae” (drop-like bumps on Descemet’s membrane) can be seen decades earlier during a routine eye exam.45
Causes and Risk Factors
FECD is primarily an inherited endothelial cell disorder. Major risk factors include:
- Genetics: CTG repeat expansion in the TCF4 gene or missense mutations in COL8A2.3
- Female sex: women have roughly double the risk.1
- Age >40 years—disease prevalence rises steeply with age.
- Positive family history—autosomal-dominant inheritance is common.
- Smoking and diabetes—associated with faster endothelial loss in some studies.2
10-Year Risk of Needing Corneal Transplant for FECD
Select your details to estimate risk factors.
Diagnosis
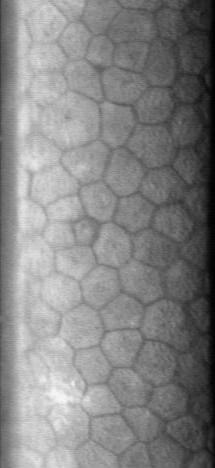
- Slit-lamp biomicroscopy shows central corneal guttae that coalesce into a classic “beaten-metal” or “orange-peel” pattern.
- Specular or confocal microscopy quantifies endothelial cell density and reveals pleomorphism and polymegathism.6
- Optical pachymetry or anterior-segment OCT measures central corneal thickness (CCT); values > 640 µm suggest stromal edema.
- Scheimpflug tomography detects posterior surface depression and irregular isopachs that predict disease progression.7
- Genetic testing for expanded TCF4 repeats may clarify prognosis in borderline cases.
Treatment and Management
Early-stage care
- Instill 5 % sodium chloride hyper-osmotic drops or ointment at bedtime to draw fluid out of the cornea.
- Use a hair-dryer on a low, arm’s-length setting each morning to speed evaporation.
- Optimize ocular surface health—treat dry eye and avoid contact-lens overwear.
Surgical options
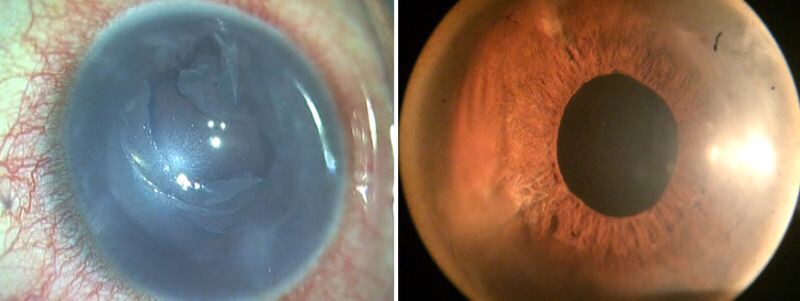
- DMEK (Descemet Membrane Endothelial Keratoplasty)—transplantation of donor Descemet’s membrane and endothelium offers rapid visual recovery and the lowest rejection risk.
- DSAEK (Descemet Stripping Automated Endothelial Keratoplasty)—slightly thicker graft but technically less demanding.
- DSO/Descemet Stripping Only + ROCK inhibitors—select patients with healthy peripheral endothelium can regenerate corneal clarity without donor tissue.
- PDEK and PKP remain alternatives when scarring or stromal disease is extensive.68
Living with Fuchs’ Corneal Dystrophy and Prevention
While FECD cannot yet be prevented, you can slow symptom progression and prepare for treatment:
- Schedule yearly exams with cornea specialists to monitor vision, cell counts, and thickness.
- Protect your eyes—wear UV-blocking sunglasses and safety goggles for home projects.
- Avoid smoking and manage systemic illnesses (diabetes, hypertension) that stress the endothelium.5
- Use preservative-free artificial tears to maintain surface comfort.
- Ask about low-vision aids such as high-contrast lighting or magnifiers if glare limits reading.
Many people maintain useful sight for years with these strategies before surgery becomes necessary.1
Latest Research & Developments
- Gene-editing trials: CRISPR-based silencing of the toxic TCF4 repeat is moving from mouse models toward first-in-human studies.9
- Descemet Stripping Only (DSO) plus ROCK inhibitors has produced 80 % corneal clearing without donor tissue in small series, lowering transplant demand.7
- Big-bubble automated DMEK devices aim to shorten operating time and expand access in community hospitals.
- Proteomic profiling shows oxidative-stress pathways activate decades before vision loss, opening doors for antioxidant therapeutics.10
Recent Peer-Reviewed Research
Survey of Topical Steroid Usage Patterns After Descemet Membrane Endothelial Keratoplasty.
Buzzi M, Collins AM, Suribhatla R, et al.
Repeat Expansion and Somatic Instability in TCF4 in Patients With Fuchs Endothelial Corneal Dystrophy Identified by Small Pool PCR.
Maeno S, Yamashita A, Oie Y, et al.
Decoding the Cornea-Glaucoma Association: Evidence From Mendelian Randomization.
de Vries VA, Szabo A, Vergroesen JE, et al.
Next Steps
If early-morning blur or glare affects daily life, ask your eye-care provider for an expedited referral to a cornea specialist. Centers that perform high volumes of DMEK/DSAEK often offer surgery-same-week pathways once donor tissue is matched. Bring recent glasses prescriptions and any prior specular-microscopy printouts to streamline the visit.
You can also connect directly with fellowship-trained cornea surgeons on Kerbside for an educational consult—no patient-physician relationship will be established—to discuss candidacy, recovery timelines, and insurance questions before scheduling locally.1
Trusted Specialists
Board-certified providers specializing in Fuchs’ Corneal Dystrophy.
