Retinoblastoma
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms and Telemedicine Consent for details.


Overview
Retinoblastoma is a rare cancer that starts in the retina—the light-sensing layer at the back of the eye. It most often affects infants and young children. Because the disease can grow quickly, early diagnosis and treatment are very important. With modern care, survival in high-resource settings is very high, and many eyes and some vision can be saved, depending on tumor size and location. Care is delivered by a team that may include a pediatric ophthalmologist/ocular oncologist, pediatric oncologist, radiation specialist, genetic counselor, and child-life and low-vision experts. 1 2
Symptoms
Retinoblastoma may be found during a routine exam or after a caregiver notices a change in one or both eyes. Common signs include:
- Leukocoria (a white or yellow “cat’s-eye” reflex in photos instead of the usual red reflex).
- Strabismus (an eye that turns in or out).
- Redness, swelling, or pain without clear infection.
- Poor or worsening vision.
These signs don’t always mean cancer, but they should be checked quickly. If you notice a new white pupil in pictures or a drifting eye, schedule an urgent eye exam for your child. 3 2
Causes and Risk Factors
Retinoblastoma begins when retinal cells develop harmful changes in a tumor-suppressor gene called RB1. About 40% of cases are heritable (germline RB1 variant); these often affect both eyes and can be passed to future children. The remaining cases are non-heritable (changes occur only in the eye). A parent may carry an RB1 variant without obvious symptoms. Because the risk pattern differs by genetics, families with a history of retinoblastoma are usually offered genetic counseling and testing. Children with heritable disease also have a small risk of a related brain tumor (pineoblastoma, sometimes called “trilateral retinoblastoma”) and a higher lifetime risk of other cancers, so informed surveillance matters. 4
Most children with retinoblastoma have no known family history. Still, prompt evaluation of warning signs (white pupil, eye turn) is the most practical way to detect disease early. 3
Retinoblastoma: Family & Symptom Risk Snapshot (Educational)
Select your details to estimate risk factors.
Diagnosis
Diagnosis starts with a dilated eye exam by a pediatric ophthalmologist or ocular oncologist. Young children often need an exam under anesthesia (EUA) for a complete look at the retina. Tests may include:
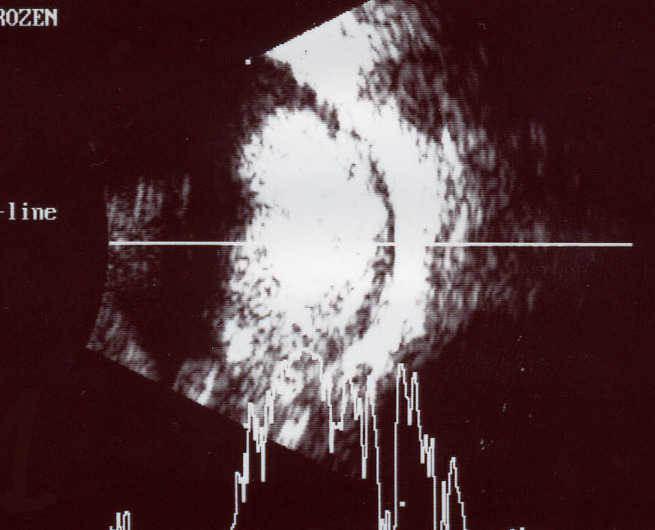
- Ocular ultrasound to look for a mass with calcification, which is typical of retinoblastoma.
- MRI of the orbits and brain to assess the optic nerve and rule out spread; MRI is preferred over CT to avoid unnecessary radiation when possible.
- Wide-field retinal imaging and documentation to track response to therapy.
Genetic testing of RB1 helps clarify whether disease is heritable and guides screening of siblings and future children. Your team will discuss any additional blood tests or imaging needed based on the stage of the cancer and whether one or both eyes are involved. 5 1
Treatment and Management
Treatment aims to save the child’s life first, then the eye, then the best vision possible. The plan depends on tumor size, number and location of tumors, whether one or both eyes are affected, and whether cancer has spread beyond the eye. Options may include:
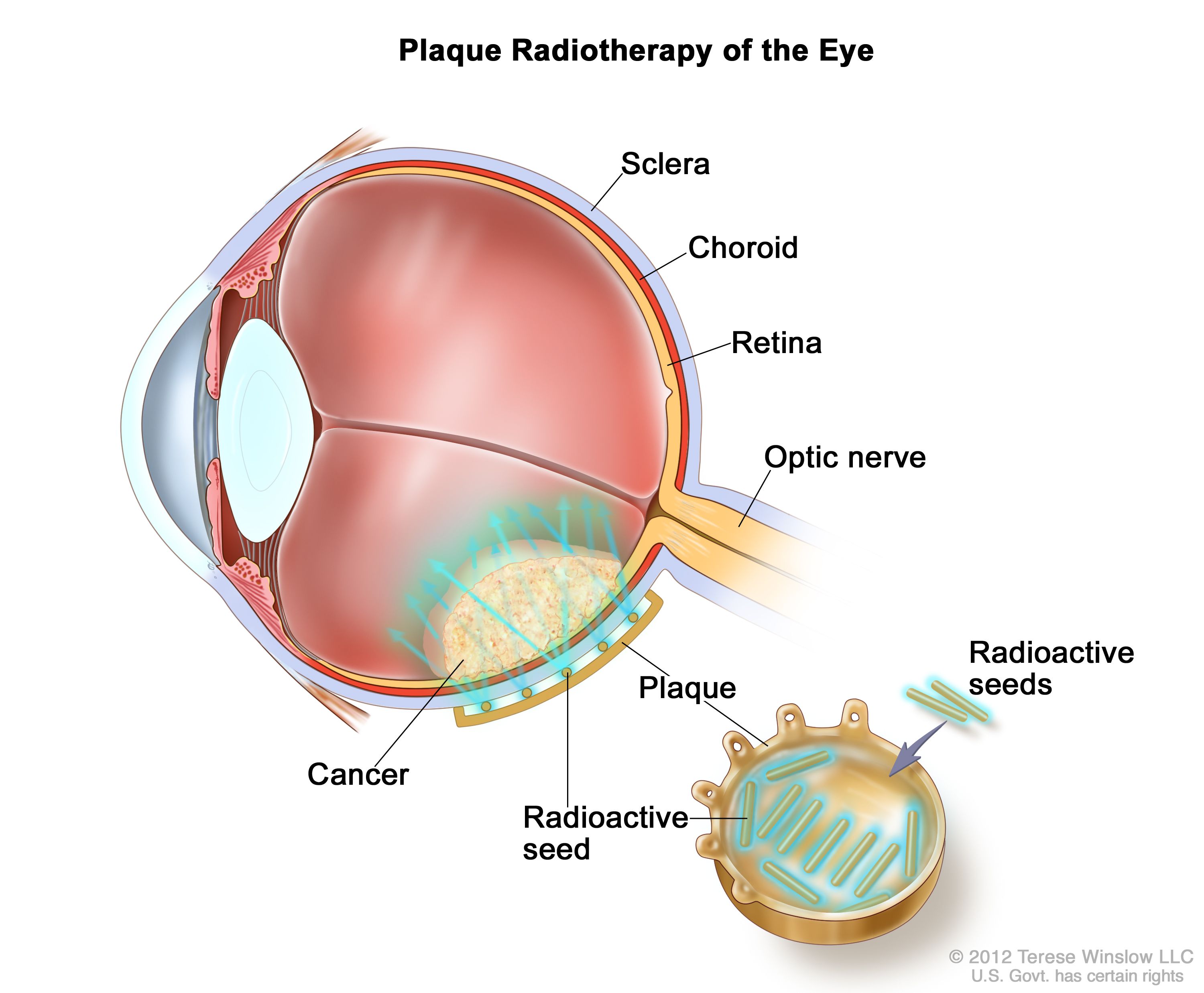
- Local therapies: cryotherapy (freezing), laser/thermotherapy, and plaque brachytherapy for selected tumors.
- Chemotherapy: systemic (IV) chemotherapy to shrink tumors (chemoreduction) followed by local treatments; intra-arterial chemotherapy (IAC, via the ophthalmic artery) or intravitreal chemotherapy for certain patterns like vitreous seeding.
- External-beam radiation: effective but used sparingly today because of long-term side effects, especially in children with heritable RB1 variants.
- Enucleation (eye removal): considered for very advanced eyes when vision cannot be saved or when safety is a concern; pathology guides whether chemotherapy is needed afterward.
Children need close follow-up during and after treatment to monitor for tumor control, new tumors in the other eye (in heritable cases), and treatment effects. Your team will also support vision rehabilitation and prosthetic fitting if an eye is removed. 4 1
Living with Retinoblastoma and Prevention
Hearing the word “cancer” about your child is overwhelming. It’s okay to ask lots of questions and to seek a second opinion at a center with ocular oncology expertise. Many families benefit from child-life services, social work, and parent-to-parent support. Vision services can help children adapt and thrive at home and school.
Practical steps:
- Keep follow-up appointments exactly as scheduled—new tumors and recurrences are most common in the first few years after treatment.
- Know your child’s genetics: if an RB1 variant is found, relatives may need testing and children often follow a tailored screening plan from infancy.
- Watch for symptoms like white pupil, eye turn, or new redness/pain and call promptly.
- Understand late effects: children with heritable retinoblastoma have higher lifetime risks of second cancers, so your team may discuss long-term healthy-living choices and targeted surveillance. 1
There’s no way to fully prevent retinoblastoma, but early detection—especially in children with a family history—can reduce complications and improve vision outcomes. 3
Latest Research & Developments
Treatment has advanced from routine external-beam radiation toward targeted approaches that limit exposure and improve eye-salvage rates. Intra-arterial chemotherapy and intravitreal chemotherapy have helped control tumors that previously required enucleation, particularly when there is vitreous seeding. Research also focuses on optimizing drug combinations, refining when to use plaque radiotherapy, and reducing late effects.
Genetic discoveries continue to shape care. RB1 testing informs counseling, sibling screening, and surveillance for pineal region tumors in heritable cases. Clinical trials are evaluating novel targeted and viral therapies for refractory disease. Ask your team whether a study fits your child’s situation. 4 1
Next Steps
If you suspect retinoblastoma—or your child was just diagnosed—here’s how to move forward:
- See the right specialist: The best first stop is a pediatric ophthalmologist/ocular oncologist. They coordinate imaging, genetics, and treatment planning.
- Collect records: Bring prior photos showing leukocoria or eye turn, any imaging (MRI/ultrasound), and reports. Ask for copies of EUAs and tumor measurements.
- Scheduling tips: Many centers require a referral. Ask about cancellation lists for faster openings. If travel is hard, request a quick review of existing records to triage urgency.
- Insurance & authorizations: Check if your plan needs prior authorization for specialized imaging, chemotherapy, or out-of-network referral to an ocular oncology center.
- Ask about clinical trials: Your team can search for open trials that match your child’s tumor pattern and genetics. 1
You can also connect with the right specialist on Kerbside for a medical education consult to understand options and questions to ask. This educational consult does not establish a patient–physician relationship.