AMD
Also known as Age-Related Macular Degeneration, ARMD
Medical Disclaimer: Information on this page is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
See our Terms for details.

Overview
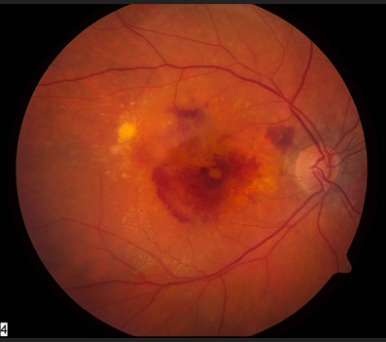
Age-related macular degeneration (AMD)—sometimes written as ARMD—is a chronic, progressive disease that damages the macula, the tiny area in the center of the retina that lets you read fine print, recognize faces, and see traffic signs. Because side (peripheral) vision is usually spared, AMD rarely causes total blindness, but it can rob you of the sharp, straight-ahead vision needed for many daily tasks. There are two main types:
- Dry (atrophic) AMD – gradual thinning of macular tissue and accumulation of drusen (yellow deposits). Accounts for about 80–90 % of cases.
- Wet (neovascular) AMD – fragile new blood vessels grow beneath the retina and leak fluid or blood, leading to scarring and sudden vision loss if untreated.
Worldwide, AMD is a leading cause of severe visual impairment in adults over 50, and prevalence is expected to rise as populations age.1 Regular, dilated eye exams are critical because early AMD is often symptom-free and highly treatable when caught in time.2
Symptoms
Early AMD may cause no noticeable symptoms. As damage accumulates, people describe:
- Blurry or fuzzy central vision, making words on a page seem washed out.
- Need for brighter light when reading or doing close work.
- Straight lines—door frames, telephone poles—appearing wavy (metamorphopsia).
- A dark, gray, or blank spot (scotoma) in the center of vision.
- Colors looking less vivid.
Symptoms can progress slowly in dry AMD or appear quickly in wet AMD. Because one eye often compensates for the other, covering each eye separately when checking vision with an Amsler grid can reveal subtle distortions sooner.34
Causes and Risk Factors
AMD develops through a mix of genetic susceptibility and environmental stressors. Key risks include:
- Age ≥ 60 years – each additional decade increases odds dramatically.5
- Family history & specific gene variants (e.g., CFH, ARMS2).
- Smoking – doubles risk and hastens progression.
- Cardiovascular factors – hypertension, high cholesterol, and obesity promote retinal inflammation and oxidative stress.6
- Race/ethnicity – Caucasian ancestry is associated with higher prevalence than African or Asian ancestry.
- Excessive UV/blue-light exposure without eye protection.
Age-Related Macular Degeneration Risk Calculator
Select your details to estimate risk factors.
Diagnosis
Comprehensive evaluation by an ophthalmologist or retina specialist typically involves:
- Dilated fundus examination to look for drusen, pigment change, or hemorrhage.
- Amsler grid self-test to detect metamorphopsia.7
- Optical Coherence Tomography (OCT) to obtain cross-sectional images and measure retinal thickness.
- Retinal imaging & fluorescein angiography to visualize leaking vessels or geographic atrophy.8
Earlier detection allows earlier intervention and better long-term visual outcomes.
Treatment and Management
No cure exists yet, but targeted therapies can slow progression and preserve vision:
Dry AMD
- AREDS2 nutritional supplements (vitamins C & E, zinc, copper, lutein, zeaxanthin) reduce risk of advancing to late disease in intermediate AMD.9
- Lifestyle changes—smoking cessation, Mediterranean-style diet rich in leafy greens and omega-3s, regular exercise.
Wet AMD
- Anti-VEGF injections (e.g., ranibizumab, aflibercept, brolucizumab) every 4–12 weeks to halt abnormal vessel growth.
- Complement inhibitors for geographic atrophy (GA): FDA-approved pegcetacoplan (Syfovre™).10
- Avacincaptad pegol (Izervay™) offers an additional option for GA with a monthly dosing schedule.11
- Occasional use of photodynamic therapy or macular laser for select lesions.
Latest Research & Developments
AMD research is advancing at a rapid pace:
- Extended-interval anti-VEGF agents and refillable drug reservoirs aim to reduce injection burden.
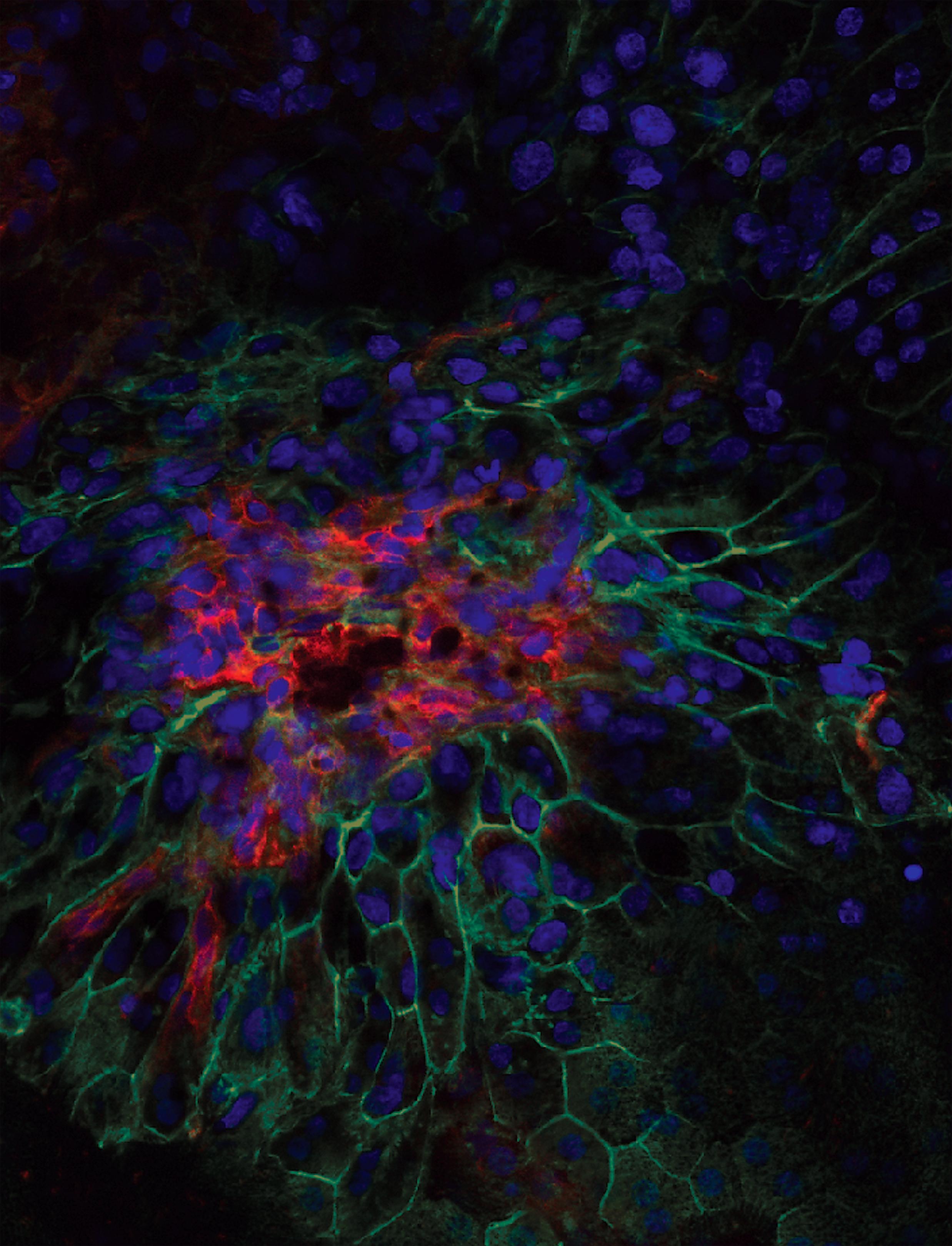
- Gene-editing and gene-replacement trials are targeting complement pathway dysregulation and VEGF over-expression.
- Complement inhibitors for dry AMD (e.g., NGM621, lampalizumab analogs) are in late-phase studies.
- Regenerative medicine—stem-cell–derived retinal pigment epithelium (RPE) transplants show promise in early human trials.
- Artificial-intelligence imaging algorithms can predict which patients will convert from intermediate to late AMD sooner, enabling prophylactic therapy.14
- Recent NEI-funded work identified ApoM modulation as a novel pathway to halt retinal cell death.15
Recent Peer-Reviewed Research
Predicting Early Onset of Age-Related Macular Degeneration: A Machine Learning Approach.
Wu E, Hasan N, Vupparaboina S, et al.
Burden and Predictors of Undetected Eye Disease in Adult African Americans: African American Eye Disease Study (AFEDS).
Dhablania N, Torres M, Burkemper B, et al.
Deep Learning Model for Automated Classification of Macular Neovascularization Subtypes in AMD.
Neri G, Rebecchi C, Oakley JD, et al.
Next Steps
Who to see: If you notice waviness, central blur, or a new dark spot, book an appointment with an ophthalmic retina specialist. They are uniquely trained to perform OCT imaging, angiography, and deliver intra-ocular injections.
How to schedule: Tell your optometrist or primary-care physician you need an urgent retina referral—especially for sudden changes. Most practices can accommodate suspected wet-AMD cases within 24–48 hours. Large centers also offer self-referral portals and tele-triage.16 National eye institutes and academic clinics (e.g., Cleveland Clinic) allow online booking or virtual visits to speed care.17
After your visit, stay engaged with your care team, follow the injection schedule (if prescribed), and explore rehabilitation resources listed above.
Trusted Specialists
Board-certified providers specializing in AMD.



